According to the popular press there is a new breast cancer cure. But we have to be careful with general statements like this. First of all, only 20% of breast cancers are HER2 positive. When the surgeon biopsies breast cancer, he sends the sample to the pathologist. Out of 100 samples, 20 come back with the finding that it is HER2 positive breast cancer.
Herceptin ® (trastuzumab), the first step of breast cancer cure
Trastuzumab is a monoclonal antibody that interferes with the HER2 receptor. Its main use is to treat HER2 positive breast cancers. But trastuzumab (brand name Herceptin ®) has serious side effects. In early HER2 positive breast cancer it can cause heart failure in 5.7–35.4% of patients, while it can cure breast cancer with a 35% cure rate of Her2-positive patients. It is significant to note that many of the studies used trastuzumab in combination with the chemotherapeutic agent anthracycline concomitantly. Anthracycline by itself has some cardio-toxic effect. Most of the studies that investigated heart toxicity of trastuzumab used this monoclonal antibody for 52 weeks. Newer studies show that as little as 9 weeks can be as effective in tumor cures, which reduces the risk of toxic effects on the heart to 2.2–2.3%.
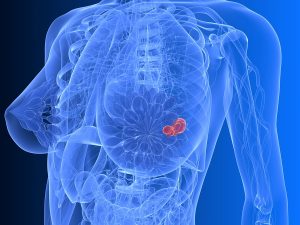
Here is a link that shows visually what the effect of Herceptin ® may be on the HER2 surface marker in a woman with this type of breast cancer.
Lapatinib (Tykerb ® or Tyverb ®), the second step of breast cancer cure
Over-expression of oncogenic receptor tyrosine kinases inhibits the absorption of aging cancer cells, called apoptosis. These are proteins that normally function to remove dying cells at the end of their life span. In HER2 breast cancer these kinases are particularly common and are responsible for the cancer cell survival. Lapatinib is a dual tyrosine kinase inhibitor, which interrupts the HER2 and epidermal growth factor receptor (EGFR) pathways. In simpler terms, it removes dying cancer cells, so they cannot reactivate the cancer or allow cancer cells to survive.
A phase 3 clinical trial was done with Lapatinib and a chemotherapeutic agent, capecitabine (brand name Xeloda ®). With combination of the two drugs there was a 51% reduction in the risk of the disease progression.
Herceptin ® and Lapatinib combined as new breast cancer cure
At the 10th European Breast Cancer Conference in Amsterdam professor Nigel Bundred reported about a trial involving 257 women with newly diagnosed, operable, HER2 positive disease. The researchers recruited these women between November 2010 and September 2015. The physicians took biopsies and the surgery followed within 2 weeks.
The trial had two parts: The physicians treated the first 130 women with trastuzumab (Herceptin ®) only, or lapatinib (Tyverb ®) only, for 11 days after diagnosis and before surgery. From other trials evidence became known that the combination of trastuzumab and lapatinib had better survival rates. The investigators decided to include a second part into their trial starting August 2013 with 127 women. Part of this trial was a combination treatment of trastuzumab and lapatinib.
Samples of tissue were taken from the original breast biopsies and then again two weeks later from the material of the breast surgery.
The pathologist examined the breast cells for a drop in the Ki67 protein, an indicator of cell proliferation. They also looked for an increase of apoptosis of 30% or more from the first date of the first biopsy. A “pathological complete response” was the term they used for a cure. When there was a partial cure, this was termed “minimal residual disease“. This meant that the tumor was less than 5 mm in diameter at the time of surgery. Women who had received the combination treatment had 11% pathological complete response (11% cure rate). 17% of the combination therapy group had minimal residual disease. There was no cure for those randomized to only trastuzumab and only 3% of that group had minimal residual disease.
Conclusion
Essentially this new research shows that two inhibitor drugs together are better than one or one in combination with conventional chemotherapy.
But we have to keep in mind that HER2 breast cancer includes only 20% of all types of breast cancer. When you hear that 11% of HER2 breast cancer was cured with the combination therapy in 11 days, it translates into only 2.2% of all types of breast cancer cured and only 3.4% of all breast cancer cases had minimal residual disease (tumor size less than 5 mm in diameter). This could be easily removed by surgery.
What everybody is excited about are the cures of 2.2% of all types of breast cancer (or 11% of HER2 breast cancer). This is a good start. But much more research is necessary to increase the number of cures. While we are seeing some progress for one group of breast cancer patients, it is not nearly sufficient to advertise this treatment as a “cure”.
For all breast cancers a more promising option is available. A study from Wayne State University, Detroit, Michigan has shown that cryoablation therapy for breast cancer without excision can give a much higher cure rate of 100% over a period of 1 ½ years. In this procedure the physician leaves the tumor in place. Cryotherapy (extreme local cold temperatures) kills the tumor cells. It gives a cosmetically superior result. The FDA accepted this alternative treatment protocol, but cancer experts are slow to accept it.