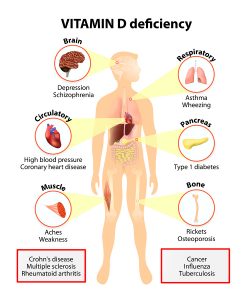
Many people supplement with 300 to 400 IU of vitamin D3, but do they take enough vitamin D3? There is a simple way of finding out: ask your doctor to order a 25-hydroxyvitamin D blood test. This will show whether the gut absorbed enough of the essential vitamin. It will also show whether or not your vitamin D3 capsules or tablets were strong enough. It is now generally accepted that a good range of the vitamin D blood level is between 50 and 80 ng/ml. Unfortunately many Americans who come down with various diseases have blood levels of less than 30 ng/ml. Here are some facts about what a lack of vitamin D3 can cause.
Increased risk of mortality with lower vitamin D levels in ICU patients
- A New England Journal study from 2009 reported about 1100 patients in Intensive Care Units (ICU). Their average vitamin D blood level was only 16 ng/ml. They tracked the mortality rates depending on the vitamin D blood level. Insufficient vitamin D levels showed an association with a mortality rate of 45%. An intermediate level had a mortality rate of 35%. And a satisfactory level of vitamin D had a mortality of only16%. Between the low level of vitamin D and the normal level there was a 3-fold difference in mortality!
- Another study from 2015 repeated the mortality study with 135 ICU patients. Researchers correlated Vitamin D blood levels with mortality rates of patients. When vitamin D levels were below 12 ng/ml, there was a mortality rate of 32.2%. Patients with higher levels of vitamin D had a mortality rate of 13.2%. The authors concluded that vitamin D blood levels were an independent risk factor for mortality. Patients less than 12 ng/ml had a 2.4-fold higher risk of dying than patients with normal vitamin D levels.
Do patients with multiple sclerosis take enough vitamin D3?
Perhaps one of the earliest results of vitamin D3 research was the following observation. More than 90% of patients with multiple sclerosis were deficient in vitamin D blood levels. Their levels were below 20 ng/ml. Other researchers showed that vitamin D could directly tone down the aggressiveness of the immune cells of MS patients. These were the ones that attacked the myelin sheath. As a result of this knowledge it is important for MS patients to take high enough vitamin D3 supplements. When they reach good vitamin D blood levels their MS is better controlled.
Canada as a northern country has 291 MS patients per 100,000 people. Contrast this to 110-140 MS patients per 100,000 people in the northern US (between the 37th parallel and the US/Canadian border). In addition south of the 37th parallel there are only 57-78 cases of MS per 100,000 people. Researchers have concluded that the less sun light people get, the higher the rate of MS in the population will be. However, instead of sun exposure you can supplement with vitamin D3 capsules to get the blood vitamin D levels up to the range of between 50 and 80 ng/ml.
Do stroke patients take enough vitamin D3?
Strokes are very common. About 6.8 million Americans survive a stroke and live with various disabilities. 15% die shortly after their stroke. 40% are left with moderate to severe disabilities. Many require special care.
- Studies have shown that patients with the lowest level of vitamin D have the poorest functional outcomes. Moreover, for every 10 ng/ml decrease in vitamin D levels the odds of a healthy recovery 3 months after the stroke fell by about half. This was independent of age and the initial stroke severity.
- In another 2015 study from South Korea 818 stroke patients took tests to evaluate whether they had adequate vitamin D blood levels. There was a clear division between those whose levels were higher than 10 ng/ml or lower. When the vitamin D level was higher, there was a 90% better recovery from their stroke after 3 months. In comparison those whose vitamin D levels were below 10 ng/ml had poor recovery rates. Experts say that vitamin D levels should stay in the range between 50 and 80 ng/ml. This will prevent numerous diseases.
Do diabetics take enough vitamin D3?
- Vitamin D3 can silence diabetes genes in connection with the right diet and cofactors of zinc and magnesium. A Mediterranean diet can stabilize the metabolism and fight inflammation. Zinc and magnesium are important cofactors in enzymes necessary to prevent diabetes. Vitamin D3 and omega-3intake are helping to control inflammation and preserve beta cells in the pancreas in diabetes patients. This is important for continued production of insulin.
- A Chinese research team found that vitamin D3 protects beta cells in the pancreas from dying off. The finding was that vitamin D3 receptors in the insulin producing cells prevented the dying off of these cells, as long as there was enough vitamin D available. Insulin production by the pancreas remained effective. And insulin is vital for long-term survival of diabetes patients. The key for diabetes patients is to take adequate doses of vitamin D3 to protect their insulin producing beta cells.
- A 2015 Italian study showed that micro vascular complications in diabetes patients were high, if the vitamin D3 blood levels were low. If patients had high levels of vitamin D3, there were no complications such as retinopathy or nephropathy. But if levels were below 20 ng/ml, damages were significant in the capillaries of the eyes and kidneys.
Do patients with inflammatory conditions take enough vitamin D3?
What do the lining of the arteries, the inflamed joints, a degenerative meniscus and heart attacks and strokes have in common? It is the inflammation that changes the body chemistry. It gets even more complicated, because the extra calories that we consume get stored as visceral fat. This is done automatically when you eat too much sugar and starchy foods. When the glycogen stores are full, any surplus sugar gets metabolized by the liver into triglycerides, fatty acids and LDL cholesterol and gets stored as body fat. The most active fat is the visceral fat between our guts and around our body organs. This produces interleukins and other inflammatory cytokines that circulate in the blood causing inflammation in all our arteries. Interleukin-6 is an inflammatory cytokine. High interleukin-6 levels contribute to causation of various cancers.
This 2015 study from Seattle University followed 218 obese postmenopausal women with a body mass index of larger than 25.0 for 12 months. Both received weight loss intervention and either 2000 IU of vitamin D3 daily or a placebo pill. Both groups lost about 5 to 10% of weight in 12 months. However, the interleukin-6 level of the vitamin D3 group had a reduction of 37.3%. This was in stark contrast to the placebo group where the interleukin-6 level reduction was only 17.2%. This type of research shows the incredible power of vitamin D3. This likely is the reason why several cancer frequencies can show a reduction with regular vitamin D3 supplementation.
Attention deficit disorder and vitamin D3
- Other research compared a group of 37 children with attention deficit hyperactivity disorder (ADHD to 37 normal children. Blood levels of vitamin D were 19.11±10.10 ng/ml in the ADHD group and 28.67±13.76 ng/ml in the normal group. Other researchers have found similar findings, establishing that very low vitamin D levels have a connection with ADHD.
- A prospective study from Spain involving 1,650 mother-child pairs investigated the effect of mother’s vitamin D level during her pregnancy with the risk for ADHD by the time the child was 4 to 5 years old. Schoolteachers followed the standard test procedures to establish the ADHD diagnosis. The study showed that for every 10-ng/ml increment of the mother’s blood vitamin D level during her pregnancy the children had 11% less ADHD-like symptoms. The authors cautioned that it takes mega doses of vitamin D3 to reach these kinds of results. The usual 400 IU of vitamin D3 per day will not achieve the desired increase of vitamin D3 levels, but amounts of 5,000 IU to 8,000 IU are necessary to achieve this.
Schizophrenia and vitamin D3
A 2014 Meta analysis found that low vitamin D levels have an association with a 2.16-times higher probability of having schizophrenia than controls with normal vitamin D levels. Another study examined whether those patients who had an acute psychosis would have lower vitamin D blood levels than schizophrenia patients in remission or control patients without schizophrenia. Studies compared 40 patients with an acute psychosis to 41 patients in remission and 40 healthy controls. Patients with an acute psychosis had extremely low vitamin D blood levels, while patients in remission had much better vitamin D levels. Healthy controls had the best vitamin D levels.
Absorption and metabolism of vitamin D3
Magnesium plays a central role in activating vitamin D3. This publication points out that magnesium is also necessary for absorption of vitamin D3 in the gut. The activation of vitamin D3 is also partially responsible for vitamin D absorption. Both vitamin D3 and magnesium play an important role in bone and calcium metabolism. The fact that every body cell has vitamin D3 receptors shows how important it is for the maintenance of the body. Many researchers say that vitamin D3 qualifies as a hormone because of the specific effects on cells via vitamin D3 receptors.
Conclusion
Vitamin D3 is an important signaling hormone and vitamin that regulates the body’s calcium absorption and is responsible for bone metabolism. Research has shown that the lack of vitamin D3 causes several unrelated diseases, like rickets, multiple sclerosis, and schizophrenia. But other diseases, where a lack of vitamin D3 was present, were diabetes, attention deficit disorder and strokes. When patients with elevated inflammatory markers take vitamin D3 their interleukin-6 levels dropped by 37.3%. To achieve this, patients needed to consume at least 2000 IU. We all should have our vitamin D blood level measured from time to time. It should be between 50 and 80 ng/ml. Too many Americans are deficient in vitamin D3 and come down with the diseases mentioned! Prevention and supplementation go hand in hand. You can prevent a lot of diseases this way.