Four diseases cause most of the deaths around the world: cancer, cardiovascular disease, chronic respiratory diseases and diabetes. This story is the news right now. 50% of the 193 UN member states that signed a treaty in 2015 are falling short of their promise. They wanted to reduce premature deaths from these diseases by 2030. But this is not happening as this story shows.
I like to review these 4 key diseases and what we can do ourselves about eliminating them. We cannot afford to wait for things to happen on a national level. Rather we need to go to the grass roots of every country and change the risk factors that cause these 4 diseases.
Cancer
First, cancer is a disease of older people, unless strong genetic factors are present. In this case even children can get leukemia, brain tumors and osteogenic sarcoma. In older people DNA mutations and DNA breaks happen more often as we age. On the other hand, if we diagnose cancer in stage 1 or 2 (in the early stages), it is quite often curable.
Oncoblot test, a cancer screening test
Probably one of the less known new criteria is the fact that there is a very sensitive cancer blood test, called the Oncoblot test (released about 4 years ago by the FDA). The latest screening test that came out of the human genome project is called the Oncoblot test. It screens for 25 of the most common cancers. And it is screening for ENOX2 proteins from cancer cells. It is a 1000 USD test in the US that health plans will not cover, but it will screen for more than 25 different common cancers 6 to 8 years before they would otherwise become clinically manifest.
If you discover cancer with this early blood test and you treat it right away, you have a good chance to live a few years longer. You may come down with another cancer down the road, but treat it early again, and you will still have a better life expectancy. Remember: four diseases cause most of the deaths, cancer is one of them!
Cardiovascular disease
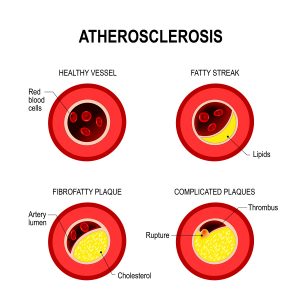
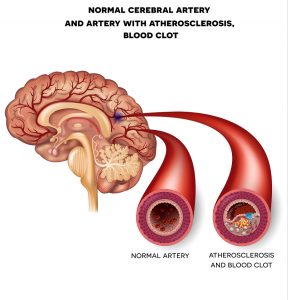
Furthermore, people develop cardiovascular disease from poor eating habits and a lack of regular exercise. There are a few percentage points of people with familiar high cholesterol. These people need to see their family doctor for a prescription to lower cholesterol. But the majority of people will do well by changing their diet into a Mediterranean diet; lose weight until their body mass index reaches a value of 21 to 24. With this diet it is important to cut out all refined sugar and starchy foods. Regular exercise in a gym will also prevent hardening of the arteries. Chelation therapy has been shown in this study to help reduce hardening of arteries.
Diabetes patients have accelerated hardening of the arteries
We know from diabetic patients who have accelerated hardening of the arteries how devastating cardiovascular disease can be. Heart attacks, strokes, kidney failure, amputations of the lower leg and blindness are just some examples. Even patients who do not have diabetes can get these complications at an older age. The key is to think preventatively, change the diet, exercise regularly and you will lower all those risks. Remember: four diseases cause most of the deaths; cardiovascular diseases belong to that group and are a major player.
Chronic respiratory diseases
There are different reasons why a person may develop chronic respiratory disease. A common disease is chronic obstructive pulmonary disease (COPD). COPD often has a link to smoking heavily as a younger person. This is where the damage to the lung tissue has started. Exposure to cigarette smoke leads to loss of elastic tissue in the bronchial tubes. The lungs have a difficult time to exhale to get rid of the CO2. The end result is that your breaths are shallow and you can’t get enough oxygen, because the lung is already filled with air.
Asthma and COPD
Another disease is asthma. Nowadays physicians can treat this condition well with a corticosteroid inhaler and salbutamol. Salbutamol dilates the airways by relaxing the muscles of the bronchial tubes. The corticosteroid keeps the lining of the bronchial tubes thin, so that the air can move in and out of the lung.
If asthma is not treated properly there can be permanent damage to the airways and the clinical picture would look similar to COPD.
With end-stage COPD patients the only therapy the physician can offer is continuous oxygen flow treatment. With power failures these machines that supply oxygen will stop working. People need to make provisions to have a back-up generator. Again, we need to remember: four diseases cause most of the deaths. Chronic respiratory diseases belong to them.
Diabetes
Patients with type-2 diabetes (Type 2 DM) are usually older than 30 years of age.
That’s why they are called “mature onset diabetes” or “adult onset diabetes”. For several decades a patient may “incubate” diabetes and have one or more of the diabetes risk factors, such as high blood pressure, obesity, high cholesterol or high triglycerides, but have normal blood sugars.
Physicians have followed patients like this for several decades in the well known Framingham Heart Study and found that a high percentage of them do come down with type-2 diabetes later in life. In the past this time of incubation was termed “pre-diabetes”. Now we call it “syndrome of insulin resistance” or “metabolic syndrome”. Diabetes belongs to the group of diseases that are associated with chronic inflammation in the body.
Causes of type-2 diabetes
Type-2 diabetes often associates with other endocrinological diseases such as Cushing’s syndrome (an adrenal gland hyperactivity) or acromegaly (increased growth hormone production). In these diseases other hormones are tilting the hormone balance by counteracting insulin thus leading to a relative shortfall of insulin, which is another cause for type-2 diabetes. There is confusion among scientists regarding possible genetic reasons for type-2 diabetes. The environment or weight gain may trigger various genetic loci that exist. The syndrome of insulin resistance has shown some connections between hypertension, obesity and type-2 diabetes.
Death in diabetics usually comes from a heart attack, a massive stroke, but it may also come from systemic infections, called sepsis. Dr. Taylor from Newcastle University showed on 30 volunteers that 43% of diabetics could be cured by a diet of 600-700 calories for 8 weeks. The medical literature also knows that regular exercise is beneficial for diabetics. It cannot be overstressed that four diseases cause most of the deaths; diabetes belongs to them and is a major player.
Conclusion
Four diseases cause most of the deaths. They were the cause of death for several years. They are cancer, cardiovascular disease, chronic respiratory diseases and diabetes. The secret is to minimize the impact of each of these diseases. You can prevent chronic respiratory diseases by stopping to smoke and treating asthma properly. To treat cancer successfully one needs to diagnose it early and remove it surgically. With cardiovascular disease chelation therapy has shown a difference. Otherwise a regular exercise program and a Mediterranean diet, which has anti-inflammatory qualities, will help. Dr. Taylor from Newcastle University demonstrated that he can treat diabetes with a low calorie diet. Each one of us has a responsibility to do something about our diagnosed condition. We cannot wait for magic cures. We need to do what has known benefits. Hopefully with these short hints will help you to improve your health.