The following article describes living with the aging process. Older adults undergo the process of aging between the ages of 50 and 80. This is a complex process affecting various systems parallel. There are hormone factors that are particularly prominent in women during menopause. Joints are affected by degenerative changes, which can lead to total knee and hip replacements. The aging process was described in an article by Monica Jimenez at Tufts University.
What is aging?
Aging is the loss of function over time. The body is much more complex than a car, so there are more possible points of failure. Christopher Wiley is a scientist on the Basic Biology of Aging Team who studies the role of nutrition and metabolism in aging at a cellular level at Tufts University. He said:” The fact that life works is amazing”. He went on to say: “The body tries to maintain itself and restore homeostasis(self-healing) even in the face of all this stress and all this damage. We have these really sophisticated programs for dealing with these points of failure.”
Aging goes on relentlessly
He explains the aging process this way: “It can start with something as simple as a broken molecule, one little thing that goes wrong in one cell, and then it’s like the butterfly effect,” Wiley said. “The tissue starts struggling, and then the organ, and then your entire body.”
Dr. Wiley warns about those who say physicians could make people “immortal”. “There’s definitely a misconception out there that we’re trying to make people immortal. But there is never going to be an immortality vaccine,” Wiley said. “There’s never going to be one thing that defeats all of aging. There’s always going to be another point of failure.”
Slowing down biological aging
The emphasis of research about aging is not to add chronological years. It is on biological aging and on how well our cells and tissues are functioning. Dr. Sarah Booth is the director of the Human Nutrition Research Center on Aging (HNRCA) at Tufts. She said: “Lengthening the time in which we can continue to move around, care for ourselves, and participate in social life and activities, is a worthier goal than extending years of suffering.” Many people become disabled in their last years of life, then they die. “Healthspan” is a new term for our years of freedom from disability, Booth noted.
Factors that prolong healthy aging
- Telomere length: One of the factors of longevity is our telomere length. Telomeres are the protective caps at the end of each chromosome. When they wear down, it leads to mistakes in the DNA copies of genetic information. There are supplements and herbs that can elongate telomeres. Exercise and the fasting mimicking diet also make telomeres longer. Older adults in good shape have longer telomeres, which stabilizes the DNA in their cells.
- Healthy diet: Researchers have determined that several diets are healthier than others. The Mediterranean diet is anti-inflammatory, so is the DASH diet, which was developed for people with high blood pressure. The HNRCA of Tufts is one of six organizations that got research grants recently to investigate life-prolonging diets. The amount was for $8.5 million.
Exercise and lifestyle factors
- Regular exercise: Over the years a lot of research accumulated data that shows regular exercise makes people biologically younger. Heart vessels have less atheromatous deposits and the brain stays younger as well. One study reported that 30 minutes of exercise daily prevents dementia.
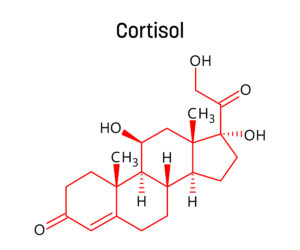
- Other lifestyle factors: other factors are whether or not you are smoking (it goes without saying that you must quit). In addition, genetics (longevity gene), the environment (polluted or not), stress levels and socioeconomic class all play a factor in how fast we age. These latter points are difficult to tease apart, but they influence us globally. Target organs for aging are: the brain, heart, eyes, and bones, along with cancer, obesity, and more.
Hormone replacement
- Bioidentical hormone replacement: One factor about delaying aging significantly was not mentioned in the review article by Monica Jimenez. But I am including it, because bioidentical hormone replacement is important for women who undergo menopause in their 50’s. I also mention it because men enter andropause in their 60’s. BiEst estrogen and progesterone cream make a big difference for the symptoms of menopausal women. Similarly, men experience a lot of relief with testosterone injections twice a week, when blood testosterone levels are low. If they have a lack of erections (erectile dysfunction) they may in addition need to take the “happy pill”. Sildenafil or tadalafil can treat erectile dysfunction by giving a good erection to a menopausal male. Hormone replacement can add as much as 10 healthy years to your life.
Discussion
Dr. Booth said: “We’re looking at the same question through different lenses with different tools, technologies, and perspectives. Progress in aging research is only going to be achieved by bringing together different disciplines addressing the same problem.”
Christopher Wiley added: “The biggest change I’ve seen in the past ten years is that we really are finding new, different ways of actually intervening somewhere that could potentially extend the healthy years of life, and prevent people from getting age-related diseases.” He mentioned that scientists are gradually reducing the suffering associated with aging: “What aging research is really trying to do is compress the morbidity and make it as small as possible – to alleviate suffering,” Wiley said. “I think that’s a much more humanitarian goal, and I think we’re having a lot of success with those efforts.”
Conclusion
Aging is a slow process that starts the moment we are born. But between the age of 50 and 80 we age faster. I mentioned 5 specific areas that can slow down the aging process. If somebody smokes, he/she must stop smoking. Cigarette and tobacco smoking the biggest aging factor. The protective caps at the end of each chromosome go by the name of telomeres. When they shorten prematurely, mistakes occur in the DNA copies of genetic information. This leads to premature aging.
What keeps you younger for longer
The good news is that exercise, the fasting mimicking diet and several supplements can elongate telomeres. A healthy diet like the Mediterranean diet and regular exercise keeps the arteries open preventing heart attacks and strokes. Bioidentical hormone replacement helps to rebalance your hormones, which is important for normal cell function. In anti-aging circles they talk about life prolongation of about 10 years for hormone replacement alone. It comes down to not simply extend your lifespan, but to extend your years of healthy living without disability.