A recent publication describes how a new multi cancer blood screening test can diagnose various cancers early. Many years back the same research group at the Johns Hopkins Medical School did lung cancer screening studies. The researchers then were analyzing saliva samples between 1974 and 1982. They identified 15 patients who later developed adenocarcinoma of the lung. The researchers were able to diagnose the lung cancer 1 year prior to what ordinary screening tests could do. This ensured an early diagnosis and early treatment with a better long-term prognosis.
Liquid biopsy promises early cancer detection
The new publication from the Johns Hopkins University in Baltimore, Maryland, is based on the following fact: Cancer cells consist of mutated cells. They shed DNA with mutations typical for this cancer into the bloodstream. By taking blood samples and analyzing the circulating mutated DNA researchers can first establish that the DNA belongs to a certain cancer mutation. But at the same time, they can locate the cancer, if they find mutated DNA. The pathologist can say that the patient has a cancer in a breast, the colon, lungs or ovaries, wherever it is located.
Oncoblot test was a precursor to the multi cancer blood screening test
Around 2014 a cancer screening test came out of the human genome project. It was called the Oncoblot test. It screened for 25 of the most common cancers. And it was screening for ENOX2 proteins from cancer cells. Apparently, this is a fetal protein normally expressed only during fetal life, bit in adults only expressed when a cell turns cancerous. It was a 1000 USD test in the US that health plans did not cover. But it screened for more than 25 different common cancers 6 to 8 years before they become clinically manifest: Suddenly around 2017 the Oncoblot test was no longer available. I could not find out the reason for this. Was the test producing too many false positives or false negatives? This would have made this cancer screening test unreliable. Apparently researchers of the Oncoblot test company are attempting to refine the test further.
My own case of prostate cancer
Strangely enough in 2016 I had an Oncoblot test done and it accurately diagnosed that I had prostate cancer. My cancer specialist from Ft. Lauderdale used Doppler ultrasound to visualize it and performed a 3-dimensional prostate biopsy to verify the histology. Subsequently he removed it with ablation cryotherapy, because a study of his involving 70 prostate cancer patients and spanning over 10 years had shown the best survival data. My 3-monthly PSA values since have been negative for recurrent prostate cancer.
New multi cancer blood screening test from Johns Hopkins Medical School
A review in Science magazine explains the details of the new multi cancer blood screening test. It is called CancerSEEK and is based on 16 common genetic markers that show changes in cancer cells. In addition, the researchers also test for cancer-related proteins, which change when cancer cells are present. The test also indicates the location of the early cancer. CancerSEEK can detect about 60% of liver cancers and 100% of ovarian cancer. The researchers tested 812 healthy controls. Only 7 (1%) tested positive for cancer. CancerSEEK also tested 1005 patients who had early cancer.
More details of the CancerSEEK test
The test detected between 33% and 98% of cases, which depended on the tumor type. The sensitivity was 69% or higher for stomach, pancreatic, and esophageal cancers; ovarian and liver cancer had a sensitivity of 98%. In 80% of the cases physicians could narrow the positive cancer test to two possible sites. The researchers think that the cost of one CancerSEEK test will be less than 500.00 USD. There is another study described where 9,911 participants were enrolled. 25 cancers were found. The diagnosis involved 2 lymphomas, 2 colorectal cancers, one appendix cancer, 2 uterine cancers, one thyroid cancer, one kidney cancer, 9 lung cancers, one breast cancer and 6 ovarian cancers. This study will continue to go on for another 5 years.
Possible problems with the new multi cancer blood screening test
Researchers dubbed the cancer screening test as “liquid biopsies” with the purpose to detect hidden cancers. The smaller the cancer is, the less the cancer cells excrete DNA and cancer proteins into the bloodstream. This means that in some of the early cancer cases the sensitivity of the test could be very small. Because many cancers will be detected much earlier there could be definite cures, if the cancer is in an early stage. On the other hand, Dr. Nickolas Papadopoulos from the Johns Hopkins University in Baltimore, Maryland, said: “The issue is not overdiagnosis, but overtreatment.” Some of the small tumors may never turn into larger tumors and it is justified to observe for a period of time.
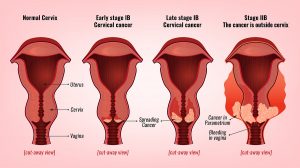
A large 5-year clinical study involving up to 50,000 women is the next project to test the CancerSEEK test further. A private philanthropic group, The Marcus Foundation, is funding this project.
Conclusion
A new multi cancer blood screening test, the CancerSEEK test, is in development. It is based on a combination of various cancer markers. Researchers measure cancer DNA mutations and also cancer proteins. They also determine the tissue location of the cancer. Researchers did much work already in terms of sensitivity and specificity of the test. Physicians integrate the test further with conventional medical tests to confirm the location of the cancer. With breast cancer mammograms are the additional tests, with colorectal cancer colonoscopies. A large 5-year clinical study involving up to 50,000 women is the next project to test the CancerSEEK test further. In future the CancerSEEK test will become a routine screening test for cancer. The cost for one CancerSEEK test will be less than 500.00 USD. The hope is that cancer cures will improve due to earlier detection.