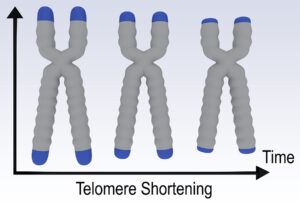
A recent publication noted that regular exercise makes you 9 years younger. The researchers meant that the biological age is 9 years younger than your chronological age. They went one step further and proved that regular exercise elongates your telomeres, which is why people who exercise regularly live longer. Specifically, they found that sedentary people had 140 fewer base pairs at the endpoints of their telomeres compared to people who engaged in regular physical activity. In other words, the biological age of a person who exercises regularly is lower than that of a sedentary person. This difference can be measured in leukocyte telomeres. With regard to the base pairs contained in telomeres the highest physical activity group showed the most elongation of the telomeres. There was a 9-year difference in terms of biological age between the highest exercise group and the sedentary group.
Other means of elongation of telomeres
Apart from regular exercise lifestyle factors can also modify the length of telomeres.
Smoking, a lack of regular exercise, exposure to stress and intake of polyunsaturated omega-6 fatty acids, especially linoleic acid shortens our body telomeres. Soybean oil, sesame seed oil, walnut oil and cotton seed oil are containing 45 to 50 % of linoleic acid, and for this reason should be avoided. The antioxidant effect of omega-3 fatty acids elongates telomeres by reducing the rate of telomere shortening. Antioxidants like vitamin E, vitamin C, beta-carotene were associated with longer telomeres and a lower risk to develop breast cancer.
A few dietary recommendations
Here are a few healthy food recommendations that will elongate your telomeres.
- Include antioxidants, fiber, organic soy protein and healthy fats (derived from avocados, fish, and nuts).
- Stay lean, active, healthy, and stress-free.
- Eat foods such as salmon, herring, mackerel, halibut, anchovies, cat-fish, flounder, flax seeds, chia seeds, kiwi, black raspberries, lingonberry, green tea, broccoli, sprouts, red grapes, tomatoes, olive fruit, and other vitamin C-rich and E-rich foods. They are a good source of antioxidants. Avoid tuna and grouper fish (too rich in noxious mercury).
- These combined with a Mediterranean type diet containing fruits, and whole grains will help protect your telomeres.
- There are certain individuals who live longer than the rest of us. They may have a certain advantage, which is a longevity gene that makes the telomeres longer. Resveratrol also works through elongation of telomeres.
Telomerase can also lead to telomere length
I attended the 22nd Annual World Congress on Anti-Aging Medicine In Las Vegas (Dec. 10-14, 2014) that dealt with telomere length and how nutrition can positively influence what our genes express. This ultimately determines how long we live. Dr. Al Sears gave one of the talks at the conference.
He pointed out that shortened telomeres are causing cells to behave like old cells. In the lab we can lengthen telomeres. Telomerase activated animals regrew their brains! In the human situation the goal is to find ways to preserve the length of our telomeres in all our key organs. Alternatively, this can also be reached by inhibiting the breakdown of the enzyme telomerase, which will lead to a lengthening of telomeres. In his research Dr. Sears found at least 123 nutrients, vitamins and natural compounds that will elongate telomeres, often by stimulating telomerase.
Lengthening of critically shortened telomeres
Testing for critically short telomeres is clinically more important than using average telomere length tests. Dr. Sears said when a patient has been shown to have short telomeres and this patient is started on telomerase stimulating supplements, telomere lengthening can be documented within one month of starting the supplementation. Acetyl-L-carnitine and resveratrol are two substances that reliably elongate telomeres.
Vitamin C and other telomerase stimulators
Vitamin C will significantly delay shortening of telomeres, which translates into delayed aging. Age-dependent telomere shortening is slowed down by enrichment of intracellular vitamin C via suppression of oxidative stress. In addition, vitamin C has recently been shown to stimulate telomerase activity in certain stem cells. There is an herb, called Silymarin extract, which was found to increase telomerase activity threefold. N-acetyl cysteine is a building block for glutathione, a powerful antioxidant. In addition, it has been shown to turn on the human telomerase gene. Other telomerase stimulators are green tea extract, ginkgo biloba, gamma tocotrienol (one of the components of the vitamin E group), vitamin D3 and folic acid. Telomerase Inhibitors from Natural Products and Their Anticancer Potential.
Conclusion
A research paper found that regular exercise makes a person 9 years younger in terms of the biological age. The underlying process is that telomeres get longer with regular exercise. Specifically, the researchers found that sedentary people had 140 fewer base pairs at the endpoints of their telomeres compared to people who engaged in regular physical activity. I listed other factors that elongate telomeres and help with longevity. When you combine regular exercise with dietary factors that also elongate telomeres, you are better off than with exercise alone.