Life expectancy between the sexes has always been different: females generally outlive males by several years, but close observation from the Office of Health Economics in Great Britain shows a shift in Life expectancy. Males have been catching up, and their life expectancy rates have been rising faster than those of females. There is still a difference for a boy born in 2002. He will have a life expectancy of 76 years, whereas his sister will live to age 81.
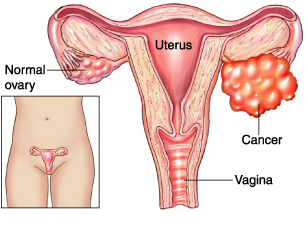
Researchers believe that the reason for the shift is lifestyle change in females. Many of them now face the same workplace stress that has been traditionally shouldered by males. Detrimental habits are also more common in females. Heavy drinking in young females has more than tripled in the last 17 years, and 10% of young females exceed the recommended drinking limit (compared to 12% males). Non-smoking campaigns are less successful in women. Males have cut their smoking habits. 51% smoked in 1974, and by 2002 only 28 % were smokers. Female smokers amounted to 41 % in 1974, but by 2002 there were still 26 % smokers. The results show most dramatically in cancer statistics. Since 1973 lung cancer rates in men have been reduced to half and the lung cancer survival rate has increased. In comparison lung cancer in females during the same time period has increased by 45%. As a result of sedentary lifestyles the body mass index has also shown an increase.
Estimates showed that by the year 2010, life expectancy will likely converge for both sexes at an age of 81.
Reference: BMJ 2005; 331:656 (24 September)
Last edited December 6, 2012