Dr. Fields gave a talk in Las Vegas about orthopedics without a knife. His talk took place at the 23rd Annual World Congress on Anti-Aging Medicine on Dec. 12, 2015 in Las Vegas. Dr. Fields gave a talk entitled “Regenerative orthopedics – non-surgical repair with stem cells/PRP/prolotherapy”. In essence the talk was about alternative treatments to surgeries in orthopedic medicine.
Dr. Peter Fields, MD, DC is a board certified medical physician and chiropractor. He is also the director of the Pacific Prolotherapy & Medical Wellness Center in Santa Monica, CA.
Introduction
Joints, muscles, tendons, ligaments and joint capsules control the movements in joints. Due to injuries and wear and tear these body parts can have a lack of function, which will lead to pain and disorders. The result can be weak, torn or damaged ligaments and tendons, arthritic changes, excessive joint motion, increased pressure, and a decrease in range of motion.
This is the common treatment cycle in medicine
Joint pain prompts you to see the doctor. You are told it is arthritis, and you get non-steroidal anti-inflammatories (NSAID’s). You come back with more pain, and you’ll get a stronger NSAID prescription. Eventually a cortisone injection is given, which helps for a few months, but then the pain reoccurs. The doctor arranges for an MRI scan. A referral to an orthopedic surgeon is likely to be the next step, and an arthroscopy (pinhole surgery) is arranged. In that case, if this does not resolve the pain, surgery like a knee replacement or hip replacement is suggested.
Common sayings when traditional medicine has nothing to offer
You may have heard some of these common sayings before. “Nothing more we can do about it!” -“I suggest you learn to live with it”- “You should never play that sport again!”- “Take these pain medications” and “The only alternative is surgery!”
The problem is, that none of these pieces of advice are really helpful. This type of approach does not treat the cause; it is directed against symptoms.
How to treat the cause?
Prolotherapy
Prolotherapy is a natural, non-surgical method to assist the body to heal torn soft tissues. It works in cases like torn ligaments, damaged tendons, cartilage, menisci or a torn labrum in the shoulder. Hyperosmolar dextrose solution is injected into the injured area. This stimulates the body’s healing forces and the body repairs what is damaged. More information is found here. In essence, prolotherapy fixes the cause, not just the effect; it heals, and it is permanent. Prolotherapy strengthens tissues, relieves pain and increases the range of motion in joints. There is 80 to 85% full pain relief and more than 80% improvement in range of motion. Prolotherapy promotes the healing of torn or damaged ligaments and tendons.
Conditions suitable for treatment with prolotherapy
Suitable conditions for treatment with prolotherapy are sports injuries, muscle tears, arthritis, tendinitis, bursitis, sciatica, TMJ problems, and fibromyalgia. Common areas treated with prolotherapy are the hip, knee, shoulder, ankle, neck, lower back and elbow. Dr. Fields showed MRI scans before and after prolotherapy treatments of ligament injuries within the knee and of shoulder ligament tears before and after treatment. Normally the physician expected these injuries to require surgery. But all that was done was one or two injections (prolotherapy treatments) with reactivation of the affected joint. There were astonishing results shown with MRI’s before and after herniated disc injuries and how they healed in a relatively short time following prolotherapy.
PRP prolotherapy
Platelet rich plasma (PRP) is a tool from regenerative medicine to amplify the healing response in connection with stem cell therapies . The lab technician takes blood from the patient and subsequently spins it down in a centrifuge. The platelet rich fraction (PRP) contains all of the growth factors, which have the healing power of the blood. The physicians combines this with prolotherapy to make healing even more successful. This is particularly useful for labral tears in shoulders, meniscus tears in knees and other localized injuries.
Stem cell prolotherapy
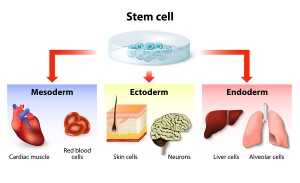
Stem cell therapy has been the gold standard for repairing more serious problems. Dr. Fields combines stem cell therapy with prolotherapy to treat more serious injuries like end stage arthritis. This is the case when bone rubs on bone, where conventional orthopedic medicine would offer a joint replacement in the hip or knee. Stem cell prolotherapy can repair any joint that has cartilage damage. A severe meniscus tear in a knee or a severe labrum tear in a shoulder would also be situations where stem cell prolotherapy is superior to surgery or to just using prolotherapy alone.
Here is a description of the procedure
Before the patient’s procedure the physician first harvests bone marrow stem cells by way of a pelvic bone aspirate; secondly the physician obtains mesenchymal stem cells from fatty tissue by aspiration of abdominal fat. A cell separator provides the stem cell fractions. The physician combines both types of stem cells, the bone marrow stem cells and the mesenchymal stem cells from fat as each one has its own strengths. These two stem cell types are more effective in combination to repair whatever tissue needs repair. Thirdly, the lab technician will draw blood from the patient to obtain PRP, which contains the growth factors needed to activate the stem cells to do their job of healing. The last step is that the physician now combines hyperosmolar dextrose (the prolotherapy part) with the stem cell preparation and mixed in PRP and injects this mixture into the injured area.
Conditions that respond to stem cell prolotherapy
This procedure has superior healing power. Before and after MRI scans of all of the major body regions showed impressive results. Several video recorded testimonials complemented the MRI scans. It is surprising how quickly and completely fairly severe injuries can heal using stem cell prolotherapy. One particularly nasty condition is osteonecrosis of the hip, which can occur as a side effect of chronic cortisone treatment for arthritis, asthma or chronic obstructive lung disease. One or two stem cell prolotherapy treatments will heal this condition because the stem cells build up brand new bone and get rid of the old necrotic bone from the osteonecrosis. Conventional medicine has no answer for this condition. Regenerative orthopedics is successful by using stem cell prolotherapy.
What are the advantages of regenerative orthopedics?
Regenerative orthopedics reduces pain very quickly and it improves function rapidly. Healing occurs naturally, and it strengthens the tissues involved. Particularly complicated lower back pains or lower neck pains (due to degenerative disc disease, facet joint osteoarthritis, spondylolisthesis and significant foraminal stenosis) respond really well to stem cell prolotherapy, getting rid of chronic pain. The speaker showed before and after MRI scans. He also shared testimonials from patients about the various procedures.
End result following stem cell prolotherapy versus conventional surgery
This is quite in contrast to what conventional orthopedics has to offer: discectomy with fusion surgery, where the patient often has scar pain later. With a laminectomy to treat a foraminal stenosis the patient may have limited improvement of the chronic back pain for a couple of months, only to experience new back pain from a subsequent spinal stenosis as a late complication from the prior surgery. The end result with conventional orthopedics is disability, pain and suffering; the end result with regenerative orthopedics is a patient that is well, active, pain free and thankful.
Conclusion
There is a form of orthopedics without a knife: regenerative orthopedics. The tools are prolotherapy for minor musculoskeletal problems. Some very conservatively minded physicians still scoff at this, but wrongly so. PRP prolotherapy is suitable for more severe injuries that require more healing power. Stem cell prolotherapy is what the physician uses for the severe cases. All of the healing power (minus the knife) is put to use. Two types of stem cells initiate healing where there is a need for it. The stem cells transform into the cell types that do the repair.
Two types of stem cells needed sometimes
Research has shown in the past that the mesenchymal stem cells alone will not heal cartilage of joints very well, but in combination with bone marrow derived stem cells this heals quite well and efficiently. Healing osteonecrosis and complicated lower neck and lower back problems borders to miraculous healing. Regenerative orthopedics is definitely something to remember should you get into trouble down the road. There are alternatives to the knife!