Marijuana was considered safe in the past, but now marijuana and uncontrolled vomiting suddenly make the news. Recently there also were reports of marijuana causing heart attacks and schizophrenia.
Abdominal pain with cannabis hyperemesis syndrome
Cannabis hyperemesis syndrome or cannabinoid hyperemesis syndrome (CHS) is a relatively new disease entity. It occurs in people who use marijuana daily for several years. But people affected by this condition often do not realize that it is an overdose of marijuana that brings on the nausea and vomiting of CHS. When they started marijuana use, they may have used intermittent doses of marijuana to treat nausea and vomiting. In intermittent doses marijuana may have been helpful, however constant use is a different story! During several years of use of marijuana, patients never had abdominal pains or vomiting, until one day CHS started.
Possible mechanisms regarding marijuana and uncontrolled vomiting
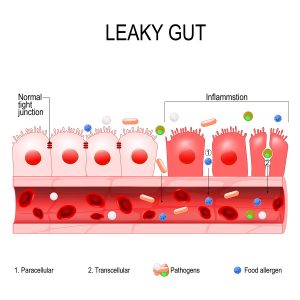
The body has its own endocannabinoid system with cannabinoid receptors that are distributed throughout the body. There are two cannabinoid receptors, CB1 and CB2. In the central nervous system, there are mainly CB1 receptors, in the rest of the body CB2. It appears that stimulation with intermittent small doses of marijuana suppresses nausea and vomiting in the hypothalamus area. However, constant stimulation of CB2 receptors in the gut with higher doses of marijuana are the cause of CHS. When a person develops cannabis hyperemesis syndrome, the only permanent cure is to stop marijuana use completely. This eliminates the CB2 receptor stimulation and allows the body to heal the gut. Researcher believe that Tetrahydrocannabinol, or THC is more powerful than the endocannabinoids. THC overwhelms the CB1 and CB2 receptors. When people who were cured of CHS restarted marijuana, their symptoms of nausea and abdominal pain returned.
In some people hot bath and hot showers help uncontrolled vomiting
Researchers noted that people reported how sometimes having a hot shower or a hot bath stopped the vomiting. The hypothalamus controls both body temperature and vomiting. A hot bath may send a signal to the hypothalamus, which interrupts the vomiting for a period of time. But with continued use of marijuana the vomiting reoccurs.
Increased strength of marihuana preparations
Dr. Wang, an associate professor of pediatrics at the University of Colorado Anschutz Medical Campus in Aurora, Colorado noted: “It’s been well documented that the amount of THC that now comes in cannabis is increasing substantially. In the ’90s the average was like 4% or 5%. Now in Colorado, it’s anywhere from 15% to 20%.” This means that THC causes more and more toxicity in patients.
In Colorado medical marijuana was legal since 2009 and recreational marijuana was legal since 2014. Dr. Wang researched the cannabis hyperemesis syndrome in Colorado. He found over 800,000 cases of vomiting in Colorado between 2013 and 2018. This was an increase of 29% from the time before marijuana became legal.
Symptoms of cannabis hyperemesis syndrome
The 5 most common symptoms of cannabis hyperemesis syndrome are continuous nausea, repeated vomiting, abdominal pain, weight loss because of decreased food intake and dehydration from fluid loss. Many people have several showers a day because it diminishes their nausea.
Three phases of cannabis hyperemesis syndrome
The cannabis hyperemesis syndrome often presents in 3 stages: the prodromal phase, the hyper emetic phase, and the recovery phase.
During the prodromal phase symptoms consist of nausea and abdominal pain early in the morning. The eating pattern is still normal in this phase. Some people increase their marijuana consumption as they hope to treat the nausea this way. This phase can last for months or years.
During the hyper emetic phase all of the 5 symptoms mentioned above can occur. This phase often continues until the patient gives up all marijuana consumption. This is when the recovery phase starts.
In the recovery phase the patient returns to a normal eating pattern. All of the symptoms gradually disappear. This phase lasts between days to months. But if the patient starts marijuana again, the symptoms return very quickly.
Treatment of cannabis hyperemesis syndrome
Patients who have severe vomiting require treatment in a hospital. The doctor starts intravenous fluids to treat dehydration. Some medicine to stop vomiting helps in the beginning. The physician must convince the patient to completely stop marijuana use, which helps to treat nausea and abdominal pain. Antacid medication like proton-pump inhibitors is useful to treat stomach lining inflammation. Frequent hot showers help to tone down nausea and vomiting. Hot showers seem to work via the hypothalamic brain center, which is responsible both for nausea/vomiting and heat perception. The physician may prescribe small amounts of benzodiazepams to treat anxiety.
By avoiding marijuana in any form THC, which is a powerful stimulus for CB1 and CB2 receptors gets washed out of the system. This allows the endocannabinoid system to rebalance itself. As long as the patient stays away from marijuana there is usually a complete recovery.
Conclusion
Since marijuana is legal in many jurisdictions the cannabis hyperemesis syndrome (CHS) occurs more and more often. Emergency teams at hospitals are kept busy treating these types of patients. It appears that CHS develops in patients who use marijuana regularly and use it in higher concentrations. Nausea and vomiting are the most common symptoms. Some patients can cope for a period of time by taking frequent hot showers. But eventually this home remedy does no longer work. A brief hospital stay may help the patient to recover from this syndrome. The patient needs to stay away from marijuana products to recover from CHS completely, otherwise there will be a relapse.