Recently CNN published an article that dealt about when stress becomes abnormal.
We all have experienced stress. It makes our heart beat faster and our breathing speeds up as well. But when the stressful situation is over, stress usually subsides also. Some people though have so much stress in their lives that they never completely recover from any stressful situation. They develop chronic stress, which can lead to physical illnesses or mental disease. I have previously written about “stress drives our lives”. In the following I am reprinting the next 5 paragraphs.
Heart attacks and strokes when stress becomes abnormal
In a 2015 Lancet study 603,838 men and women who worked long hours were followed for an average time of about 8 years with respect to heart disease or strokes. All of the subjects were free of heart attacks and strokes when they entered into the study. There was a total of 13% more heart attacks in those who worked extra hours in comparison to those who worked 40 hours per week or less. With respect to strokes there were 33% more strokes in those who worked long hours. Researchers noted a dose-response curve for strokes in groups with various workloads. Compared to standard working hours there were 10% additional strokes for 41-48 working hours, 27% for 49-54 working hours and 33% for 55 or more working hours per week.
Stress drives some of us to substance abuse
In order to cope with stress many of us “treat” daily stress with alcohol. It makes you feel good subjectively, but it can raise your blood pressure causing heart attacks and strokes down the road. A low dose of alcohol may be healthy, but medium and high doses are detrimental to your health.
Next, many people still smoke, although scientists have proven long time ago that it is bad for your health. It can cause heart attacks, various cancers and circulatory problems leading to leg amputations.
Overeating is another common problem. Comfort food relieves stress, but it causes us to put on extra pounds. As you know it is easier to put weight on than to take it off. Being overweight or being obese has its own problems: arthritis in the hips and knees makes walking more difficult. The metabolic syndrome sets in, which is a characteristic metabolic change causing diabetes, high blood pressure, heart attacks, strokes and certain cancers. The more weight you carry, the less likely you are to exercise. This can lead to further deterioration of your health.
Diabetes can occur when stress becomes abnormal
Stress causes too much cortisol secretion from the adrenal glands. This raises blood sugar, and when chronic can cause diabetes. In addition, unhealthy eating habits in an attempt to cope with stress can cause weight gain. Insulin resistance causes high blood sugars and diabetes.
Korean immigrant study
In a 2012 California study 148 adult Korean immigrants were examined. They all had elevated blood sugars confirming the diagnosis of type 2 diabetes. They had an elevated waist/hip ratio.
A high percentage of the study subjects had risk factors for type 2 diabetes. This included being overweight or obese and having high blood glucose readings. 66% of them said that they were feeling stressed, 51% reported feeling anxious, 38% said they were feeling restless, 30% felt nervous and 3% said they were feeling hopeless. It is easy to see the connection between stress and disease!
Australian study showed that anxiety can cause diabetes
An Australian long-term follow-up study computed risk factors for developing type 2 diabetes. Stress was a major contributor to diabetes.
A 30-day episode of any anxiety disorder had a 1.53-fold risk to cause diabetes. A depressive disorder had a 1.37-fold risk to cause diabetes and posttraumatic stress disorder had a risk of 1.42-fold to cause diabetes.
Infertility may develop when stress becomes abnormal
Stress changes hormones in women causing ovulation problems and infertility. 1 in 8 couples in America have problems getting pregnant. Physicians identified stress as at least one of the contributing factors. But in men stress can also reduce sperm count and semen quality as this study describes.
Alzheimer’s disease and stress
A 2010 study from Gothenburg University, Sweden examined 1462 woman aged 38-60 and followed them for 35 years.
Psychologists assessed the stress score in 1968,1974 and 1980. 161 females developed dementia (105 Alzheimer’s disease, 40 vascular dementia and 16 other dementias). The risk of dementia was higher in those women who had frequent/constant stress in the past. Women who had stress on one, two or three examinations suffered from higher dementia rates later in life. Researchers compared this to a group of women who did not have any significant stress. Specifically, dementia rates were 10% higher after one stressful episode, 73% higher after two stressful episodes and 151% higher after three stressful episodes.
Hormone system affected by stress
I have written an article before about how stress affects our hormone system.
I am reprinting excerpts from this here (the next 4 paragraphs).
Dr. Andrew Heyman gave a talk about how stress affects our hormone system. He presented his talk at the 24th Annual World Congress on Anti-Aging Medicine (Dec. 9-11, 2016) in Las Vegas that I attended. It was entitled “Understanding the Stress, Thyroid, Hormone Connections & Prioritizing Systems”.
Dr. Heyman emphasized in particular that there is a triad of hormonal connections that is important to remember: the thyroid hormones, the stress hormones (adrenal glands) and the pancreas (insulin production). It seems like we need a balance of these hormones for optimal energy production and circulation. Under stress our sugar metabolism can markedly derail, we develop obesity and fatigue. But when balanced, we experience vitality and wellbeing.
Metabolic activation pathways
Dr. Heyman projected a slide that showed the metabolic activation pathways. Likewise, he stated that a number of different factors could influence the hormone system:
- Diet: trans fats, sugar, too many carbs, food allergies.
- Drugs: drug-induced nutrient depletion (over-the-counter drugs, prescription drugs).
- Physical exercise: frequency and type matters.
- Environmental exposure: chemicals, pesticides, herbicides, heavy metals, plastics, molds, and pollens.
- Stress: physical stress, psychogenic stress.
- Genetics: methylene-tetra-hydro-folate reductase enzyme deficiency (MTHFR mutation), APOE genes, lack of vitamin D
- Disease: past or present conditions, active disease or syndromes.
Target areas within your system
The target areas in your system are the
- Pancreas, where blood sugar can rise because of insulin resistance. In particular, too much insulin production causes inflammation, hormone disbalances, kidney damage, and hardening of the arteries through plaque formation.
- Thyroid gland, which depends on TSH (thyroid stimulating hormone) for activation. Autoantibodies can also affect it negatively.
- Brain: decrease in serotonin resulting in anxiety, depression and food cravings; decreased melatonin causing sleep disturbances; increased ghrelin and decreased leptin secretion leading to overeating and obesity.
Other target areas of stress
- Liver/kidneys: both of these organs are important for detoxification; the liver produces thyroid binding globulin, which when increased can lower the free thyroid hormones.
- Immune system (gut, lymph glands): the Peyer’s patches in the gut mucosa produce a large portion of the immune cells; lymph glands, the bone marrow and the spleen supply the rest. A leaky gut syndrome can affect the whole body, in addition causing inflammation and autoimmune reactions.
- Hypothalamus/pituitary/adrenal glands: this is the main axis of the stress reaction. A brain under stress activates the hypothalamus. It sends a cascade of activating hormones via the pituitary gland and likewise activates the adrenal glands. Finally, this leads to cortisol overproduction, and release of epinephrine and norepinephrine from the center of the adrenal glands. High blood pressure, anxiety, heart palpitations, arrhythmias and more can finally develop from this.
Treatment suggestions to cope with stress
There are thyroid supplements that can support the function of the thyroid gland. Similarly, there are several supplements to support the adrenal glands.
Chromium, vitamin D, magnesium, alpha-lipoic acid, fish oil and others are useful to support the pancreas. Relaxation methods like self-hypnosis, meditation, yoga, Tai-Chi and others are very useful to counter stress. If you can change your job to evade stress, take the opportunity and find another job with less stress. See a health professional and discuss what you can do to become more stress-resistant. If you are overweight or obese, see a dietitian to help you lose weight. Aerobic exercises like running for 30 minutes on a treadmill can help reduce stress. Various relaxation methods mentioned earlier also can counter stress. They help you to block out worrying about the past and the future, but instead focus on what is positive in the present.
Conclusion
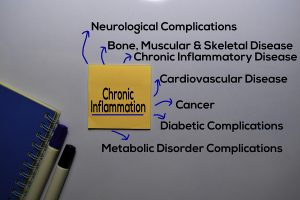
I have described what stress can do to your body. It can give you heart attacks and strokes. Stress in some people can lead to substance abuse. It can cause diabetes, infertility and even Alzheimer’s disease. I described how thyroid hormones, insulin and brain hormones are interconnected and suffer with stress. Other factors can make the effects of stress worse or better as I discussed in detail. Treatment of stress-induced conditions requires a combination of preventative steps and medical therapies. Ignoring stress is not an option as this could lead to premature death. Managing stress, as mentioned before, and keeping it to a minimum is the answer.