Unusual presentations of the Covid-19 coronavirus were unknown when it first emerged in Wuhan, China at the end of 2019. Initially the virus presented with a high fever, cough, tiredness, sore throat and aches and pains. Subsequently cases of diarrhea, conjunctivitis, headaches and loss of smell were often accompanying the illness. Patients with a weak immune system in old age or from chronic diseases are particularly vulnerable. They can come down with viral pneumonia, which often results in intubating the patient. 50% of these cases may recover, the other 50% die.
Descriptions of unusual presentations of the Covid-19 coronavirus
In the last few months doctors have seen unusual presentations of the Covid-19 coronavirus. There were cases that seemed to be fine in the first 10 days. But then sudden severe illness struck. In one case a 38-old man was diagnosed with Covid-19 coronavirus in an urgent care clinic. He was told to go home and isolate. He felt not too bad, but had a bit of a cough. The following day he woke up with his legs feeling cold and numb. His leg muscles were so weak, he could not walk. An ambulance took him to the Westchester Medical Center in New York.
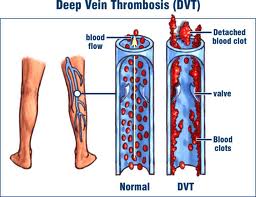
Blood clot secondary to Codid-19 coronavirus
Tests showed that he had a large blood clot in his aorta right at the bifurcation of the iliac arteries. When no blood goes through the iliac arteries, no blood can reach the femoral arteries. This explained his leg symptoms. Emergency surgery removed the blood clot and saved this man’s legs and life.
Other unusual presentations of the Covid-19 coronavirus
Apart from blood clots of all sizes doctors also found kidney failure, heart inflammation and complications of the immune system. One of the doctors stated that the virus can present in one patient as difficulties to breathe. But in another patient, there can be suddenly multi-system organ failures. Doctors noted that coronavirus can infect the lining of blood vessels directly. This causes an acute inflammation and blood clots. As blood vessels supply all organs with blood, it is not difficult to imagine that a reduction in blood flow can cause multi-organ failures. Doctors have stated that this is a confusing picture, and it will take some time to understand this further. There is another coronavirus-linked syndrome that is worrisome, the pediatric multisystem inflammatory syndrome. It is commonly found in children less than 5 years of age.
Pediatric multisystem inflammatory syndrome
This syndrome can affect children less than 5 years of age, although in the beginning it was assumed that children would be less likely to have Covid-19 coronavirus infections. Pediatric multisystem inflammatory syndrome is the second phase of a coronavirus infection. Symptoms include abdominal pain, gastrointestinal symptoms and inflammation of the heart. Symptoms are persistent fever, inflammation and poor function in one or more organs. Some children present with shock. These children need admission and treatment in a pediatric ICU ward right away. Some doctors think that the cytokine storm initiated by the Covid-19 coronavirus is responsible for this syndrome. It may be an overreaction of the immune system that can be the cause.
Delirium in patient testing positive for Covid-19 coronavirus
A patient in Saudi Arabia who has been traveling abroad presented with confusion from a delirium. He had a spiking fever and mild respiratory symptoms. A swab test for SARS-CoV-2 was positive. He recovered very quickly and spontaneously and had no residual problems.
Unusual presentations of the Covid-19 coronavirus in elderly patients
In a study from French Switzerland coronavirus patients who were older than 70 years of age were analyzed. Half of the patients who died were over 83 years old. Symptoms can be as vague as “altered general condition”, unusual fatigue or delirium. Even a fracture can be an indication that a hidden coronavirus infection caused dizziness, loss of balance and a fall.
Gastrointestinal symptoms common in adults
In adults symptoms of fatigue, diarrhea, nausea and vomiting are common for Covid-19 coronavirus. This is in contrast to the usual presentation of upper respiratory symptoms followed by a fever and coughing.
Unusual presentations of the Covid-19 coronavirus in pregnant women
A publication from Wuhan, China reported about pregnant women shortly before and after their deliveries.
Their gestational age was between 38th weeks to 41st weeks. Prior to their delivery they had no fever or symptoms of coronavirus. Following the delivery many had a mild fever of 37.5℃-38.5℃. Kidney and liver functions were normal. Two women had mild elevation of heart enzymes. The newborn babies were all healthy. Women before the delivery tend to not have any fever. After the delivery low-grade postpartum fever or mild respiratory symptoms were the only symptoms present in those with positive tests for Covdi-19 coronavirus.
Conclusion
There are unusual presentations of the Covid-19 coronavirus. Older people may present with an “altered general condition”, unusual fatigue or delirium. In very young children the pediatric multisystem inflammatory syndrome may present as abdominal pain, gastrointestinal symptoms and inflammation of the heart. On the other hand, in more severe cases acute shock may be present. In late pregnancy shortly before delivery the pregnant women had hardly any symptom and no fever. But post-delivery women with positive Covid-19 test presented with a mild fever and cold also show mild respiratory symptoms. In middle aged adults sudden blood clots stemming from inflammation of the lining of blood vessels can shut off the blood supply to multiple organs. This causes a dangerous condition of multiple organ failure. The liver, heart and kidneys are often affected.
This is still a new virus, and researchers do not know enough. Much more research is necessary to clarify the differences of presentation in patients with Covid-19 coronavirus.