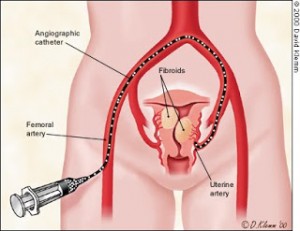
Uterine fibroids are the most common uterine tumors that affect women in North America. At least 25% have the symptoms that point to a diagnosis of fibroids, and as many as 77% may have fibroids that are asymptomatic. Symptoms of fibroids can be a feeling of fullness in the pelvic area, heavy periods and bleeding between the periods resulting in anemia. Infertility and miscarriages can also be a consequence.
About 60% of women with fibroids will undergo surgery, but the trend is moving towards nonsurgical treatment. 40% of fibroid patients will receive uterine artery embolization (UAE).
The advantages are significant, reports Dr. Sanjoy Kundu, a radiologist at Scarborough General Hospital in Toronto. Compared to the less invasive UAE, fibroid surgery has a higher rate of major complications like infection and pulmonary embolism. None of the patients undergoing uterine artery embolization experienced any complications of infection or pulmonary embolism. UAE patients also have shorter hospital stays ranging from 1 to 4 days, whereas surgical patients had hospital stays ranging from 2 to 25 days.
Due to these positive findings, 60% of treatments for uterine fibroids at Scarborough General Hospital are now done exclusively with the less invasive procedure, and researchers suggest that UAE for the removal of fibroids should become first-line therapy.
More information about fibroids: http://nethealthbook.com/womens-health-gynecology-and-obstetrics/abnormal-vaginal-bleeding-common-menstrual-abnormalities-2/abnormal-uterine-bleeding/fibroids/
Reference: The Medical Post, April18, 2006, page 16
Last edited Nov. 1, 2014