Every new parent has the wish to stimulate infants in healthy development. Children’s programs are plentiful, whether they involve gymnastics and dance or toddlers play. It is no surprise that swimming classes are also offered, and parents are not only looking at the water fun but also at water safety. They want the best for their baby and make use of swim groups that are offered for babies and infants.
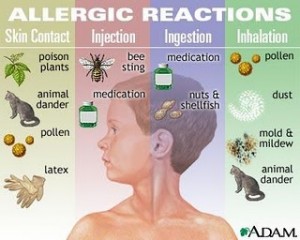
It turns out that it may be better to hold off on putting baby into swim classes at the public indoor pool. The water is fine, but the chlorination is the problem. It is common to see a irritation of the eyes due to chlorination, but data reported in the June issue of Pediatrics described findings from a group of 341 school children age 10 to 13, 13% of whom had participates in infant swimming programs point to damaging effects on the respiratory organs. Among others the respiratory condition of these children was assessed. The infant swimming group had signs of so-called Clara cell damage and changed permeability of the lining of the lung. The group that had been enrolled in infant swim groups also had significantly elevated odds of having chest tightness, physician-diagnosed asthma and exercise-induced airway constriction. The problems were aggravated even more, if the children were exposed to parental smoking.
The researchers conclude that infant swim practice in chlorinated indoor swimming pools is associated with airway changes, which along with other factors can predispose children to the development of asthma and recurrent bronchitis. More research is recommended to examine the effects of chlorination products on the infant respiratory tract.
More information on asthma: http://nethealthbook.com/lung-disease/asthma-introduction/
Reference: http://www.ncbi.nlm.nih.gov/pubmed/20075053 : Voisin C, Sardella A, Marcucci F, Bernard A.: ” Infant swimming in chlorinated pools and the risks of bronchiolitis, asthma and allergy.” Eur Respir J. 2010 Jul;36(1):41-7. Epub 2010 Jan 14.
Last edited November 2, 2014