Dr. Mark Rosenberg gave a talk on prevention of telomere shortening. This was presented at the 24th Annual World Congress on Anti-Aging Medicine (Dec. 9-11, 2016) in Las Vegas that I attended. The detailed title was: “The Clinical Value of Telomere Testing”.
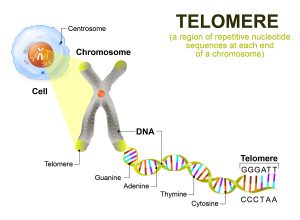
What are telomeres?
Telomeres are the caps at the end of chromosomes. They are very important in the aging process. Prematurely shortened telomeres are linked closely to all major diseases like cardiovascular disease, cancer, diabetes and more. Telomeres are also a measure of the aging process. Aging occurs due to a decrease of the number of cells in organs and/or because of a lack of functioning of these organs. Telomeres get shortened every time a cell divides. But when the telomeres are used up, there comes a time when cells can no longer divide. These cells become senescent cells or they enter apoptosis (programmed cell death).
The senescent cells can become a problem when they get transformed into cancer cells and their telomeres lengthen again. These cancer cells divide rapidly and this can become the reason why cancer patients to die.
What is the significance of telomeres?
Telomere dysfunction is the first sign that the telomeres are getting shorter in a person compared to the average telomere length in a comparable age group. This is not only important for aging, but also has clinical implications. The shorter telomeres are, the higher the risk for cardiovascular disease. Telomere length also provides prognostic information about the mortality risk (risk of dying) with type 2 diabetes and for many cancers. Many physicians incorporate a telomere blood test into periodic health checks, if the patient can afford it.
Interventions that help telomere length
Here are a number of things we can do to lengthen our telomeres.
- Rosenberg mentioned that the strongest effect on telomere lengthening comes from caloric restriction and weight loss. 80 years ago they showed at the Cornell University that rats put on calorie restriction had a 30% increase in their mean and maximum lifespan. Many research papers have confirmed that the same is true in man and that the common denominator is telomere lengthening.
- Next are regular physical activity, meditation, reduction of alcohol consumption and stopping to smoke.
- Taking antioxidants and omega-3 fatty acids regularly will also lengthen telomeres.
- Improving one’s dietary pattern by adopting a Mediterranean type diet that contains cold-pressed, virgin olive oil.
- Telomerase activators. Here is some background on the TA-65 telomerase activator, which is based on Chinese medicine. A one year trial was completed with 250 units and 1000 units of TA-65 per day. The lower dose (250 units) showed effective telomere lengthening, while the placebo dose did not. The 1000 unit dose did not show statistical significance.
Should you wish to take TA-65, only take 250 units per day, not more.
Cancer and telomeres
There is a strong correlation between cancer and telomere shortening. When cells are at the brink of dying toward the end of their life cycle the telomeres get shorter and shorter. This is the point where the cells can turn malignant. Certain genetic abnormalities help the malignant transformation, like 11q or 17q deletions or a p53-dependent apoptosis response. Once cancer cells have established themselves they activate telomerase in 85% of cases. In the remaining 15% of cancer cases telomeres are activated through telomerase-independent mechanisms. Here are a few examples.
CLL
CLL stands for chronic lymphocytic leukemia. It is a disease of the aging population. At age 90 people’s bone marrow cells have a telomere length of only 50% of the length at birth. This is the reason that in older age CLL is more common. Researchers observed a population segment and found that the shorter telomeres were, the poorer the overall prognosis and overall survival for CLL was.
Lung cancer
Researchers examined the telomerase activity in patients with non-small cell lung cancer. When telomerase activity was present, the 5-year survival was only 55%. When telomerase activity was absent, the prognosis was 90% survival after 5 years.
Prostate cancer
- Prostate cancer risk correlated with telomere shortening in stromal cells. Men with shorter telomere length in stromal cells had a 266% higher risk of death compared to men with normal telomere length.
- Another study took blood samples and determined the telomere length in lymphocytes (the immune cells). Those men who came down with prostate cancer within a year after they had their blood sample, had short telomeres. The risk for prostate cancer in these patients was 355% higher than in the prostate cancer negative controls.
Yet another study looked at surgical tissue samples from 596 men that
Underwent surgery for clinically localized prostate cancer. Patients whose samples showed variable telomere lengths in prostate cancer cells and shorter telomeres compared to prostate samples with less variable telomere length and longer telomeres had a much poorer prognosis. They had 8-times the risk to progress to lethal prostate cancer. And they had 14-times the risk of dying from their prostate cancer.
Breast cancer
Breast cancer is diverse and consists of cases whose origins are genetic (BRCA1 and BRCA2), but there are also cases where the cancer is local or has a higher stage. In families with mutated BRCA1 and BRCA2 telomeres are significantly shorter than in spontaneous breast cancer. Increased telomerase activity in breast cancer cases is directly related to how invasive and aggressive the breast cancer is.
- In one study researchers analyzed blood leukocytes in 52 patients with breast cancer for telomere length versus 47 control patients. Average telomere length was significantly shorter in patients with a more advanced stage of breast cancer than in early breast cancer. Mutated HER patients had the shortest telomeres. It follows from this that checking for the HER status and blood telomere testing adds to the knowledge of potential cancer development and prognosis.
- In patients with with larger breast tumors, more lymph node metastases and more vascular invasion the researchers found short telomere length of the cancer cells.
- More aggressive breast cancer cells have higher telomerase activity. More than 90% of triple negative breast cancers have short telomeres.
CNS disorders and telomeres
Dr. Rosenberg presented evidence for a correlation between shorter telomeres and the development of dementia. But dementias with Lewy bodies and Alzheimer’s disease are also linked to short leukocyte telomeres. The length of blood telomeres predicts how well stroke patients will do and how people with depression will respond to antidepressants.
Cardiovascular disease and telomeres
The renin-angiotensin-aldosterone system controls our blood pressure and keeps it constant. When this system is not stable, our blood pressure shoots up and causes cardiovascular disease. This is tough for the heart, as it has to pump harder against a higher-pressure gradient. A study of 1203 individuals was examining the connection between leukocyte telomere length and renin, aldosterone and angiotensin II activity. It concluded that oxidative stress and inflammatory responses affect the telomere length of leukocytes and that the more stress there is in the renin-angiotensin-aldosterone system, the more cardiovascular disease develops. The conclusion of the study was that the overall cardiovascular stress leads to shortening of leukocyte telomeres.
Conclusion
Telomere length testing from a simple blood test will become a more important test in the future as hopefully the cost comes down (currently about 300$). It can predict the general aging status by comparing a single case to the general telomere length of the public. But it can also predict the cancer risk, risk for mental disease and cognitive deficits (Alzheimer’s disease). In addition your cardiovascular status correlated globally with this test. What are the options for the patient, if the test comes back with short telomeres?
It allows you to change your lifestyle and adopt a healthy diet. You can exercise regularly, take antioxidants and meditate. There are even telomerase activators that are gradually becoming more known. They lengthen the telomeres. The cost of telomerase activators will likely still be a problem for some time. All in all telomere length tests are here to stay, but healthy lifestyle choices are the only tool for effective intervention at this point. This is good news: healthy lifestyle choices like non-smoking, exercise and avoiding non-processed foods are either free or have a reasonable price tag. Telomerase activators are big business and at this point not really affordable!