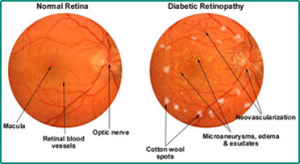
This outline is about “inflammatory marker linked to blindness”. Up to now age-related blindness or “age-related macular degeneration” (AMD) as it is medically called, has been a mystery. Notably, the retina is the light-sensitive area of the eye similar to the film in a camera. Specifically, the “macula” is that part of the retina that has the highest visual acuity. It is important to realize that several studies have been conducted lately regarding age-related blindness. Most compelling evidence sheds more light on this important health hazard of old age. One day these studies might even lead to a cure or powerful preventative measures to avoid AMD from ever developing.
Macular degeneration related to C-reactive protein
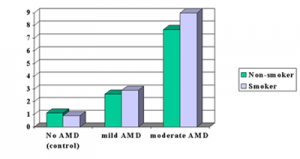
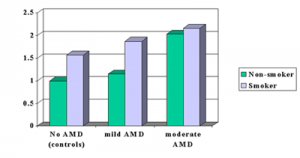
Particularly, one such study is the one by Dr. Johanna M. Seddon and co-workers published in the Feb. 11, 2004 issue of the Journal of the American Medical Association. Almost 1000 patients with various degrees of age-related degrees of blindness from the Age-Related Eye Disease Study (AREDS) were classified by the degree of their macular degeneration. As an illustration, I have produced the bar graphs below based on these studies.
Details of AMD in relation to CRP
For one thing, the researchers defined four groups, namely those with no AMD who served as controls. The second group were those with mild AMD, the third group those with moderate AMD. And the fourth group were those with severe AMD who were legally blind. Specifically, they suspected that an inflammatory marker in the blood stream of these patients, called C-reactive protein (CRP), might be present in the more severe cases of blindness when compared to the control group who did not have any inflammatory changes in the macula. Indeed, the bar graphs below show exactly what the test results indicated. Another key point, they also found that smokers (blue bars) tended to have slightly worse blood tests in terms of CRP (more inflammatory substances circulating in the system) within the same severity category of the age-related eye changes.
| CRP (mg/L) Levels in Various Degrees of Severity of Age-related Macular Degeneration (AMD) |
Risk of AMD depends on value of CRP
The investigators studied the risk for the highest percentile of the CRP tests within various subgroups of AMD. They found several differences as shown in the next table. First there was a low probability to develop AMD in a person with a normal looking macula. The investigators took this risk as the 1.0 point for comparison. In contrast a person with a normal looking macula who smokes has a 1.5-fold risk of developing AMD later. Patients with a moderate degree of AMD have about a 2-fold risk of getting a severe degree of AMD. This is true for smokers and non-smokers. Once the inflammatory cycle has started, the process of causing a moderate degree of AMD is so strong. This means that the effect of smoking will not add that much in comparison.
This is the first study of this kind that established that CRP is useful as a screening for the risk to develop AMD. Physicians already use CRP as a test for monitoring progress in rheumatoid arthritis or to monitor for the risk of developing a heart attack or stroke.
AMD risk studied by another research group
Another study by Dr. Johanna M. Seddon and co-workers was published recently in the Archives of Ophthalmology. 261 people aged 60 years and older with established AMD were followed for 4.6 years and checked for deterioration. 101 patients had deterioration of their AMD.
| Risk of Developing Age-Related Macular Degeneration (AMD) in Highest CRP Percentile |
 |
Omega-3 fatty acids protect against AMD
The authors analyzed the patients’ diet habits and found that increased fat intake was a high risk factor for deteriorating AMD. Both vegetable and animal fat had a 2-to 3-fold increased risk for deterioration of the AMD to a more severe stage (legal blindness). Fish, omega-3 fatty acid and nuts had a protective effect, but only when omega-6 fatty acid (linoleic acid) intake was low in the same group. The studies showed that the risk of age-related blindness was reduced by 40% when patients ate nuts at least once per week. The authors concluded that a “fat conscious diet” would be good for “maintaining good eye health” and at the same time be beneficial for prevention of heart attacks and strokes.
The authors will do further studies to investigate potential ways of helping patients with AMD and to understand the mechanisms of the disease process better.
References
1. JAMA 2004;291:704-710 2. Arch Ophthalmol – 01-DEC-2003; 121(12): 1728-37