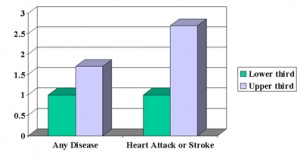
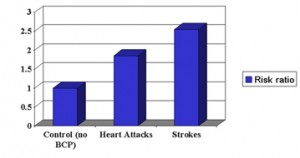
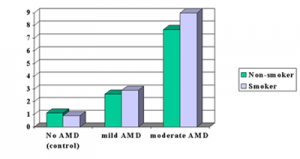
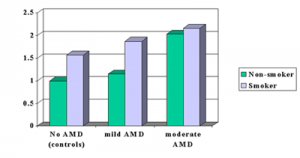
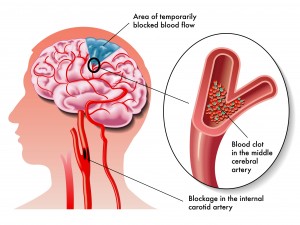
A 12 year prospective, well controlled follow-up study from Finland determined that uric acid blood tests are not only useful in following patients with gout or kidney stones, but are also predictive for future health problems including death. Dr. Leo K. Niskanen from Kuopio University in Finland and colleagues followed 1,423 middle-aged Finnish men who at the beginning of the study were free from cancer, heart disease, strokes and diabetes. After about 12 years the researchers found that 157 men had died, 55 from heart disease or strokes. When men with elevated uric acid levels were classified into low, medium and high levels, an interesting observation was made when subclasses were compared with each other. Those men in the upper range of uric acid levels had a risk of more than 2.5-fold to die from a heart attack or stroke when compared to men with uric acid levels in the lower range. Also, men in the higher range were 1.7-fold more at risk to die from any cause than men in the lower range of uric acid levels.
Dr. Niskanen said that uric acid simply seems to be another good marker for spotting troubles in health. The mechanism of this connection is not known at this point in time, but the test is easy to do and is very useful in screening a middle aged population.
| Risk of Developing a Heart Attack or Stroke with Elevated Uric Acid Blood Test |
Other investigators in the past have also observed a similar association, but this seems to be the first longterm and prospective study.
More info on:
1.heart attacks: http://nethealthbook.com/cardiovascular-disease/heart-disease/heart-attack-myocardial-infarction-or-mi/
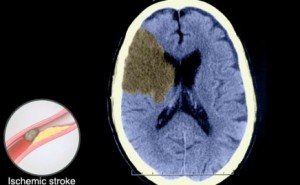
2. strokes: http://nethealthbook.com/cardiovascular-disease/stroke-and-brain-aneurysm/
3. Gout: https://nethealthbook.com/gout/
Reference: Arch Intern Med 2004;164:1546-1551
Last edited October 26, 2014