A new report from the CDC (Center of Disease Control) in the US has revealed that up to 40% of premature deaths could be prevented by simple lifestyle changes. As this link shows every year about 900,000 premature deaths occur in the US, which are due to 5 major diseases that in the opinion of the CDC can be prevented by 20 to 40%. Here are the diseases that kill: cancer, heart disease, COPD/emphysema, stroke and accidents/injuries. These conditions were responsible for 63% of all deaths in the US in 2010.
Let’s discuss each of these conditions and how one could lower the risk of dying from them.
1. Cancer:
The Framingham Heart Study has shown that smoking and cancer are closely related. Smokers who quit can significantly reduce their risk of getting cancer. We also know that exercise and prophylactic supplements like fish oil and vitamin D3 have cancer preventative effects.
Antioxidant supplementation that included beta-carotene, vitamin A, vitamin C, and vitamin E daily or on alternate days for 1 to 12 years, along with selenium supplementation reduced the incidence of cancer of the esophagus, colon, pancreas, stomach or the liver. Insulin resistance due to sugar and starch overconsumption is causing cancer, particularly breast cancer, colorectal cancer and endometrial cancer. I have discussed this in a recent blog.
Pollution has been linked to increased lung cancer risks as discussed here.
2. Heart disease:
Heart disease can be caused by several factors in combination. Lifestyle issues are important: Smokers need to quit smoking as the Framingham Heart Study has shown more than fifty years ago that smoking causes heart attacks. Obesity and diabetes also contribute significantly to the risk of heart disease. Often these are connected to faulty nutrition, which is another lifestyle issue that comes to mind when too much sugar and starchy foods are taken in; your liver will convert these into fatty acids, triglycerides and elevated, oxidized LDL cholesterol, which gets deposited under the lining of the arteries. A lack of exercise adds to this problem as a lack of exercise lowers the protective HDL cholesterol and fat is deposited under the lining of the arteries. Start exercising and your protective HDL cholesterol will rise, your total cholesterol to HDL ratio will lower to healthier levels and your risk for hardening of the arteries and for getting a heart attack will fall. If you have diabetes, it is important that you manage your blood sugars well; this means that if you inject insulin, you want the blood sugar tests to be within the normal range and the hemoglobin A1C values to be below 5.5%. Poorly controlled diabetes is an important cause of heart attacks and strokes. High blood pressure is also an important cause of developing heart attacks and strokes. It is important to control your blood pressure by taking blood pressure lowering pills and also by exercising regularly. Exercise seems to send a signal to relax the blood vessels thus lowering the blood pressure, which in turn prevents heart attacks.
3. COPD/emphysema:
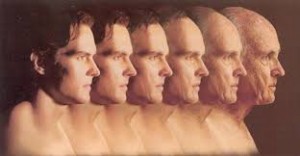
Chronic obstructive pulmonary disease (COPD) or emphysema is mostly caused by chronic exposure to cigarette smoke from smoking. The earlier you can quit, the better your chances that your breathing will not be the limiting factor when you age. But it is also important to avoid exposure to other noxious gases, such as from welding and from exposure to pollution. This may involve a decision to move to a less polluted area. Or it might involve a job retraining. Those who are suffering from COPD can be helped to a certain extent by a portable oxygen tank with nasal prongs.
4. Stroke:
As mentioned before, quitting smoking, controlling high blood pressure and controlling blood sugar, if you suffer from diabetes have been shown to stabilize your blood vessels including the ones that supply your brain. The key is to prevent hardening of the arteries by a healthy lifestyle. Exercising and keeping your weight under a body mass index of 25.0 have been shown to be effective stroke prevention. Healthy nutrition as indicated above under “heart disease” is equally important for stroke prevention. Go green (eat more vegetables, consume more green smoothies), cut down grains, sugar and starchy foods and you will live longer without strokes and heart attacks. Remember, what’s good for your heart is good for your brain!
5. Unintentional accidents/injuries:
Wearing helmets when bicycling, wearing seat belts when driving in a car, avoiding risky behaviors are all measures that save lives. One factor stands out in all of this: if you drink too much, you run the risk of being involved in unintentional accidents or injuries. People may not like to hear this, but your brain lacks the natural inhibitory impulses when you are under the influence of alcohol, so you become more daring and you may not pay attention for the split second that could have prevented an injury or accident. People react very differently to alcohol. Some people feel inebriated after only ½ a glass of wine or beer whereas others can drink more before they make mistakes. The best is to be sober when you drive, ski, use power tools or walk in traffic. Even climbing ladders requires a clear mind!
Conclusion:
As the CDC said 20 to 40% of premature deaths (deaths that occurred before the age of 80) could have been prevented, if the above-mentioned recommendations were followed. Let me rephrase this: 180,000 to 360,000 premature deaths every year in the US before the age of 80 could have been prevented! Curative medicine cannot help with these statistics as a heart attack or stroke has happened when it has struck you. Cancer and end stage lung disease are similar conditions that you are suddenly faced with when they occur and unintentional accidents just seem to happen. This is where the importance of prevention can be seen, because these little baby steps every day are adding up to something formidable, a force to be reckoned with. Be part of the solution, think prevention!
More information on:
1. Cancer mortality: http://nethealthbook.com/cancer-overview/overview/cancer-mortality-rate/
2. Higher vitamin D3 intake lowers mortality from heart attacks, strokes, cancer, fractures due to osteoporosis: http://nethealthbook.com/news/higher-vitamin-d-levels-associated-lower-risk-mortality/
Last edited Nov. 8, 2014