Introduction
Phage therapy against superbugs is the latest concept in treating infections. Antibiotic resistance has developed into a huge clinical problem. Every year in the US about 2 million people have infections from antibiotic resistant bacteria, and 23,000 people die as result of it. Certainly, there is a desperate need to find alternative treatment options to treat antibiotic resistant infections. One such option is to use phages, a specific form of viruses to treat antibiotic resistant bacteria. Here is a scientific overview regarding the use of phages for the treatment of antibiotic resistant infections.
History of phages
The observation of phages attacking bacteria goes back more than 100 years. The French Canadian microbiologist, Félix Hubert d’Herelle (1873–1949) described in 1917 what bacteriophages are. He also coined the term of “phage therapy” for the treatment of bacteria with phages. Dr. d’Herelle recognized phages to be virus-like organisms that attacked bacteria and could kill them. When Fleming detected antibiotics, phage research came to a halt. Drug companies invented more and more antibiotics, as it was easier to kill bacteria this way. But now with emerging resistances of bacteria to antibiotics, there is a sudden revival of the 100-year old research on phages. The problem is that there has not been much clinical experience with phage therapy against super bugs until lately. In 1923 Dr. d’Herelle co-founded the Eliava Institute in what is now Tbilisi, Georgia. This institute has the world’s most comprehensive database on phage therapy in man.
Two clinical examples of phage therapy against superbugs
Chronic prostatitis due to superbug
Pranav Johri, a Canadian of Indian descent was suffering of a chronic prostate infection. Physicians had used five different antibiotics, but all to no avail. His doctor told him that he had a chronic prostatitis problem for which there was no cure. But Pranav saw another specialist who determined that Pranav had a prostatitis due to a superbug, which was resistant against all the common antibiotics. Pranav traveled to the Eliava Institute in Tbilisi, Georgia. He paid 6000.00 CAD and had three treatments. After the first treatment his temperature became normal for the first time in months, and his chronic pain subsided. He and his wife were so excited that they felt like celebrating. They did sightseeing, went out to restaurants and enjoyed their travels, all things he was unable to do for months. Pranav had finally received a cure with phage therapy to his chronic prostate infection.
Enteric infection due to superbug
Tom Patterson who had visited Egypt in 2015 together with his wife fell ill on the last night of his holiday. Eventually he went into a hospital in his hometown, San Diego. The doctors told him that he would likely die. He had acquired a multi-antibiotic resistant infection. He was slipping in and out of consciousness. His wife, Steffanie Strathdee, an infectious disease epidemiologist, remembered having heard about phage therapy during a virology class during her training in Toronto. Tom received two separate phage cocktails that two separate research teams in the US had prepared for his condition. He received the first dosage into his abdomen.
Intravenous phage therapy
The second administration was intravenously. There are only a handful of patients who had received treatment with phage therapy in the US; he is probably the first one who received phage therapy intravenously. A few days later he woke up. He had to relearn basic life skills like swallowing and speaking. But he made a full recovery from a serious disease with multi-antibiotic resistant bacteria. The University of California San Diego School of Medicine had helped Tom to recover from his illness. They announced at the end of June 2018 that they would be opening the Center for Innovative Phage Applications and Therapeutics in San Diego.
Modern phage technology
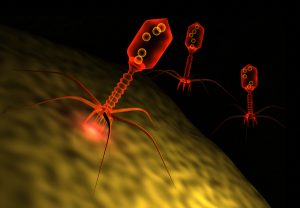
Basically phages are viruses that specialize in killing bacteria. They exist in nature wherever bacteria grow and help that they do not over-proliferate. But they can be useful in fighting difficult to treat bacterial infections as well, like pseudomonas ear infections, Clostridium difficile gut infections or Methicillin-resistant Staphylococcus aureus infections in skin wounds. In the former Soviet Union and in the Eliava Institute in Tbilisi, Georgia, extensive phage research has accumulated valuable data over decades. In the West physicians relied on the power of antibiotics, and phages stayed on the back-burner of the research lab.
Genetic engineering of phages and toxins produced by phages
Combining phage research and genetic engineering research we are entering a new era of manufacturing biological compounds that can kill bacteria similar to antibiotics. Here is a review article of this new exciting field. I only include this link to show that researchers are now getting a handle on phages. They can be genetically modified to specifically attack one kind of bacterium. The DNA of the phage can be isolated and injected into bacteria. I do not expect you to understand all of what is discussed in this link.
Conclusion
As a result phages are more and more in use to treat difficult chronic infections where bacteria have become resistant to multiple antibiotics. It requires a team of experts who are familiar with phage cocktails. The cocktail is a careful combination of various phages that will fight the antibiotic resistant infection.The composition of it has to be according to the bacteria present in the patient’s bacterial flora. As shown with two clinical examples very sick patients can recover relatively quickly from their chronic infections. After this breakthrough more and more centers for phage therapy will open and this should help reduce the death rate from antibiotic-resistant infections.