This review is about how to cope with time switches. In Europe daylight saving time begins on the last Sunday in March and wintertime starts on the last Sunday of October. Here in North America we start daylight saving time on the second Sunday of March and end it on the first Sunday of November each year.
With the time switch just last weekend I thought it would be worthwhile to comment in a blog how our bodies, particularly our hormones suffer from this.
You may have heard about the circadian rhythm with respect to hormones. The changes of the sun causing the day/night cycle have profound influences on our hormones, called the diurnal hormone changes or the circadian rhythm.
How do circadian rhythms work?
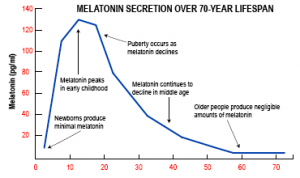
In the morning when you open your eyes, light enters our eyes and the hypothalamus registers this in the suprachiasmatic nuclei (see Ref.1). There are also links from the hypothalamus to the pineal gland, where melatonin is synthetized and stored. The light signal stops the secretion of melatonin from the pineal gland, although it is still being produced during the day in the pineal gland, but stored there until the evening hours set in. You may have noticed that you start yawning when the light dims in the evening. That’s when melatonin is released into your system to let you know its time to go to sleep.
Of course, we have electrical light and can turn night into day if we choose to! This works for a limited time, but eventually tiredness sets in, and melatonin wins the upper hand. Melatonin is the master hormone of the circadian rhythm.
Cortisol and melatonin are natural opposites
It is interesting to note that cortisol does exactly the opposite. Cortisol is the adrenal gland hormone that helps us cope with stress. When we are fully awake, we need cortisol to cope with stress. Melatonin inhibits cortisol secretion and cortisol inhibits melatonin secretion, so they are natural opponents working together for your common good. This is part of the circadian rhythm. We can measure these hormones and this is how researchers have found out how this works.
Time switches affect the circadian rhythm
When we switched time back by one hour on our wristwatch and clocks, the internal time in our body did not accept that right away. The body needs to gradually adjust to this by reading the external signals: when are we opening our eyes? What is the light intensity when we get up, what is the light intensity when we go to sleep? Some people find it easy to adjust; others find it very difficult to adjust. Some individuals breeze through the adjustment process in a day or two. For others it can as much as 1 or 2 weeks before the hormonal adjustment is completed.
Symptoms of problems adjusting the circadian rhythm
Symptoms due to time switch are a feeling of hangover on the first one to two days after the switch. This is despite you having gotten enough sleep, but the quality of sleep was not the same as before the time switch. Your head feels heavy, you are irritable, and you may feel mildly depressed. You also may find it more difficult to concentrate on one thing and you experience fatigue. Some experience insomnia. What is behind this is a disturbance of your cortisol levels. Your cortisol level is normally highest in the early morning hours, just before you wake up. As a male your testosterone level is also highest when you wake up thanks to the circadian rhythm. Both cortisol and testosterone recover their hormone storage during your deepest sleep.
Our hormones are linked to the internal diurnal clock
In women the ovarian hormones have not only a monthly rhythm, but also a 24-hour diurnal rhythm, based on the internal 24-hour clock. The hypothalamus and the pituitary gland have an intimate involvement in both sexes regarding this diurnal rhythm. They are in communication with the pineal gland that produces melatonin to regulate all of the major hormone systems. So, when we switch our watch back by one hour in the fall or forward by one hour in the spring, our body clock is out of sync with the new time that rules the world. This state of being out of sync may last for a few days. We still get tired according to the old time and we still wake up according to the old time until our internal clock has readjusted. People have genetic differences on how quickly they readjust.
Jet lag
When we travel eastward or westward through time zones a phenomenon of being “out of sync” occurs as well, very similar to what happens with time switches. It is the same re-adjusting process of the internal circadian rhythm that our bodies have to come to terms with. Some people are affected more when they travel west though time zones, and it may take them longer to adjust to it compared to traveling east. But other people complain that for them it is just the opposite, and traveling east is the problem for them. North-south travel does not cause jet lag as the internal time and the external time remain synchronized. A very similar phenomenon is happening with the spring and fall time switches. Some people find it nervier when in spring the clock is advanced by one hour and others complain that fall is their difficult time when the time is switched back by one hour. There are genetic differences of how we adjust with our internal clocks.
Shift workers
Shift workers experience problems with the circadian rhythm as well. The switch between working day shifts and night shifts leads to a condition called “shift-work sleep disorder” (Ref.3). Similar to jet lag this is due to the fact that there is a disruption of the synchronization between the body’s inner clock and external cues. The work rules do not allow enough time for recovery. It would be much more cost effective, if unions and employers allowed those who are naturally born to cope with night time shift to work those shifts and allow those who are sensitive to shift-work sleep disorder to work only day shifts. We live in an age of political correctness, but we tend to overlook how our bodies work.
What you can do to ease yourself into the time switch
1. As there is a lack of deep sleep with the time switch, it is not a bad idea to take a short nap when you feel tired during the day. Catch a nap on the weekend or on a day, when you are off work! It’s good for you! This will build up your adrenal gland hormones and give you the extra surge of energy you are craving for.
2. At the end of the day though, you need to go to bed according to the new time to train your pineal gland and your entire hormone system about the new time situation. Your body needs the cues from you, when you start and end your day, so that it can sync your internal clock with the outside time.
Melatonin restores the circadian rhythm
3. A simple remedy that fits right into your hormone rhythm is to take a melatonin tablet (about 3 mg for an adult), available at your health food store or drugstore 30 minutes before bedtime. Ref. 2 states that melatonin “restores the circadian rhythm “. This helps your circadian hormone rhythm by giving it an evening boost of melatonin. This tells your system it is time to go to sleep. At that time when you close your eyes the signals through the optic nerve shut down. This gives the circadian rhythm yet another signal about what time it is. In just a few days (for very sensitive people in 1 to 2 weeks) your entire hormone system including the circadian 24-hour undulations will be reset. Now your internal clock has been reset and is in sync until the next time switch.
More about hormones: http://nethealthbook.com/hormones/introduction-hormones/
References
1. Melmed: “Control of Hormone Secretion” in: Williams Textbook of Endocrinology, 12th ed.Copyright 2011 Saunders, An Imprint of Elsevier
2. Rakel: Integrative Medicine, 3rd ed. Copyright 2012 Saunders, An Imprint of Elsevier
3. Daroff: Bradley’s Neurology in Clinical Practice, 6th ed. Copyright 2012 Saunders, An Imprint of Elsevier