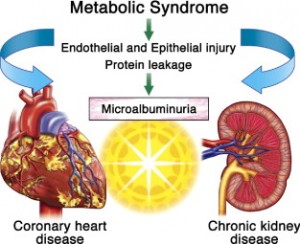
In a review article for physicians from the St. Michael’s Hospital of the University of Toronto (see reference below) Dr. Monge outlined some of the newer human research where links were found between the lining of the blood vessels and the hormones produced by fat cells that lead to the complications of the metabolic syndrome. In obese people there is a cluster of conditions such as high blood pressure, high blood sugar, high cholesterol, lipid abnormalities and high insulin levels, which is known as “metabolic syndrome”. Another name that was used for this condition in the 1990’s was “syndrome of insulin resistance”.
Dr. Monge pointed out that blood vessel health depends on the fine balance between two opposing forces. On the one hand there is a system that leads to blood vessel spasm, blood clotting, growth promoting, inflammation causing and oxidizing. On the other hand there is a system that is responsible for blood vessel relaxation, growth inhibition, blood clot dissolving, inhibiting inflammation and antioxidant activity. Complex changes occur in our metabolism when we put on pounds and accumulate too much fat. It is important to realize that fat is not just sitting there, but is composed of highly active fat cells that respond to insulin and growth factors and in turn produce a number of hormones and factors that affect the cells that are lining the blood vessels. Inflammatory cytokines are produced by fat cells that attack the blood vessels by producing atheromatous plaques, causing them to accumulate fat again and help in the processes that lead to rupture of the plaques.
The end result is that the deadly interplay between the fat cells and the endothelial cells lining the blood vessels tips the balance between the two systems mentioned above to the point where heart attacks and strokes suddenly occur.
There are two complex pathways that are involved in this process and that are linked to what was stated above. One crucial aspect of this involves nitric oxide, a small molecule that is normally produced by the endothelial lining cells and that is needed for normal circulation of the heart muscle, skeletal muscles and internal organs. This protective system is where much of the derangement of normal metabolism occurs with regard to the metabolic syndrome.
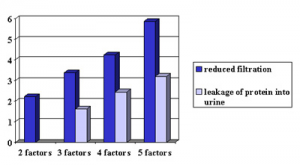
Dr. Monge pointed out that with these newer insights into the complex metabolic changes associated with the metabolic syndrome in obese people, there will be very practical results in the near future. Anti-inflammatory medications are already being utilized and some of the anti-diabetic medications have been shown to reduce the risk of heart attacks. It is hoped that sensitive tests will be developed to measure the hidden endothelial dysfunction at a time when preventative steps are still effective or early intervention can be done.
More info on the metabolic syndrome: http://nethealthbook.com/hormones/metabolic-syndrome/
Reference: Metabolic Syndrome Rounds (April 2004): J.C. Monge “Endothelial Dysfunction and the metabolic syndrome”
Last edited Oct. 26, 2014