A new study describes that sleep training to prevent insomnia and depression is desirable. Notably, the study published in JAMA Psychiatry took 291 people age 60 years and older and followed them for three years. In this case half the participants received treatment with sleep training, the other half treatment with cognitive behavioral therapy. The other half was the control who received sleep education therapy from a public health educator. It is important to realize that both groups received 120 minutes weekly group sessions for two months. That is to say, following training of 2 months the subjects were followed for 36 months. It must be remembered that they completed monthly questionnaires to monitor for depression and insomnia. At the end of the study almost 1/3 of the cognitive behavioral group still were free of insomnia.
The control group who received sleep education therapy initially showed no longer any
improvement. In other words, the initial progress did not last with sleep education only. The study was also published in CNN.
Results about rates of depression
Those subjects of the cognitive behavioral therapy group who had a sustained remission of their insomnia disorder had a rate of 82.6% less depression. This was in comparison to the subjects who did not sustain their treatment against insomnia. Dr. Pim Cuijpers commented that the results of the study show “a completely new and innovative way” of tackling the growing problem of depression. Dr. Cuijpers is a professor of Clinical Psychology at the Free University of Amsterdam.
A brief background about depression in older patients
Depression is common in people above the age of 60. About 30-50% of this age group develop depression. Part of this could be that older people often do not get enough sleep as middle-age or younger adults do. Melatonin production declines with older age and this may play a role in insomnia of older people. On the other hand, one of the major symptoms of depression is a lack of sleep. It seems that a lack of REM sleep, the deep sleep that makes us dream, is responsible for both troubles, sleeping (insomnia) and depression.
Cognitive behavioral therapy administered by a therapist is effective for insomnia
It is important that a therapist administers the cognitive behavioral therapy. There are recordings available online that provide cognitive therapy, but they are not individualised. Dr. Irwin said: “That’s why CBT-I is so effective in person, because the therapist is helping that individual navigate and negotiate with themselves — and it can be really hard work,” Irwin added. “I believe that’s also why CBT-I apps or online tools often don’t work — people get frustrated, disappointed or angry at themselves, and they basically stop the work.”
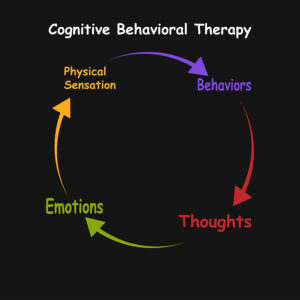
The rationale for cognitive behavioral therapy (CBT)
CBT for insomnia has five components: Stimulus control, sleep restriction, sleep hygiene, relaxation and cognitive behavioral therapy. Researchers gave the program the name CBT-I. Sleep hygiene and relaxation involve these sleeping habits: going to bed at the same time every day, eliminating noise and blue light from electronic devices. Also, you want to keep your bedroom cool, take warm baths and do yoga for relaxation.
Stimulus control and sleep restriction
Stimulus control involves getting out of bed, if you can’t sleep. Dr. Irvin said: “Most people stay in bed, fretting about not falling asleep, which then turns the bed into a negative space. Instead, people are taught to get up after 10 minutes of tossing and turning, do quiet, non-stimulating activities, and not to come back to bed until they are sleepy.” Sleep restriction means that a person lies in bed only to sleep plus 30 minutes. It is a way to make people with insomnia get out of bed instead of lying there awake.
Cognitive behavioral therapy
Cognitive behavioral therapy disrupts irrational thoughts and beliefs about sleep. Patients with insomnia often think “I can never sleep” or “I might die if I don’t sleep tonight.” A therapist has training to help the patient find a way back to a more realistic mindset. Eventually the patient accepts the bed as a welcoming place.
Cognitive behavioral therapy is effective in preventing depression
Dr. Irwin pointed out that chronic insomnia often leads to depression. A dangerous consequence of depression can be preoccupation with suicide. A certain percentage of patients with depression in any age group want to kill themselves. This is where cognitive behavioral therapy can intervene and make a huge difference. As mentioned earlier almost 1/3 of patients who received cognitive behavioral therapy for two months retained their normal sleep pattern. It was among this group that 82.6% had no depression compared to a control group. These are very important statistics. Dr. Irwin said: “We have shown that we can actually target insomnia with cognitive behavior therapy and prevent depression from occurring”.
Conclusion
A new study in JAMA Psychiatry describes that sleep training to prevent insomnia and depression is feasible. Sleep researchers used cognitive behavioral therapy sessions for two months on subjects who suffered from insomnia. The treatment group had profound effects with respect to improving insomnia and depression. Almost 1/3 of subjects treated with cognitive behavioral therapy returned to a normal sleeping pattern. And this subgroup of patients had 82.6% less depression. The lead author, Dr. Irwin thinks that cognitive behavioral therapy could become the new way of how to treat and prevent depression.