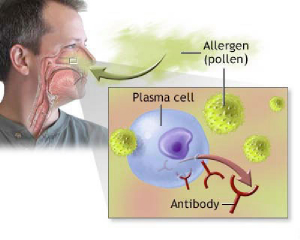
Seasonal affective disorder (SAD) does have its grip on people who react to a lack of sunlight in the winter month. As a result depression in the winter season is not uncommon. Some people just report it as feeling “down” and “tired” or report a lack of energy. Despite all the reports about SA, epidemiological studies have shown that the rate of depression is not the highest in dreary months like January or February but it spikes in the months of April and June. Dr.Teodor Postolache, a psychiatrist at the University of Maryland made a recent presentation at a meeting of the American Acadamy of Allergy, Asthma and Immunolgy delving into the reason for this finding. He compared the exposure of tree pollen which triggers a cytokine release to a tsunami.Virtually no outdoor allergens are present in the winter months, but with the release of tree pollen people who are vulnerable to allergies are exposed to massive amounts of allergens. The released cytokines may affect brain function and behaviour, resulting ultimately in changed cortisol levels and an altered serotonin metabolism. After breathing the cytokines are already released in the nose and they can continue their action in the prefrontal brain area where the centers for mood, anxiety and impulsivity are located. Dr. Postolache and his colleagues confirmed that individuals with a history of allergy and asthma had a 2.5 fold of suicide compared to controls and those with allergic rhinitis had a 1.7 fold higher risk.
For the first time it could also be demonstrated that cytokine levels in suicide victims were significantly elevated in the orbitofrontal cortex, the brain area that affects mood. Intranasal corticosteroids in the form of nosedrops can bring significant relief to allergy sufferers, and Dr. Postolache and his team will examine the benefits of intranasal corticosteroids closer in a clinical study. Whereas systemic corticosteroids have shown a negative impact on mood disorders and depression, the local application of a nasal spray or drops is geared to abolish the pathways from the nose to the brain for the inflammatory cytokines.
More information on seasonal rhinitis: http://nethealthbook.com/ear-nose-and-throat-diseases-otolaryngology-ent/nose-problems/allergic-rhinitis/
Reference: The Medical Post, April 1, 2008, page 1, 34
Last edited November 3, 2014