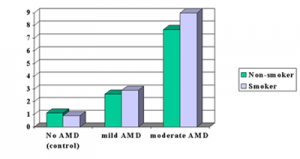
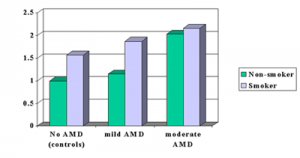
Age related macular degeneration (AMD) is one of the more frequent reasons for loss of vision in the ageing population. The disease is also the most prevalent reason for blindness in developed countries.
A group of researchers from the Netherlands made it their mandate to investigate, in which proportion antioxidants were useful in the prevention of AMD. Supplementation with vitamins C, D and E was used and also beta-carotene and zinc. The observations were made using questionnaires from the Rotterdam Study (1990-1993).
The group on which the research concentrated consisted of inhabitants 55 years of age or older living in a middle class suburb of Rotterdam. Of 5836 at the baseline with a risk of AMD 4765 had reliable data of their dietary habits. At the end of the study 4170 participated in the follow up.
Dietary intake of vitamin E and zinc was inversely associated with the development of AMD: the group with an intake of vitamin E and zinc had less macular degeneration than those whose diet was deficient. A higher than median intake of all the four nutrients, vitamin E, zinc, vitamin C and beta-carotene showed even more benefit. The risk to develop macular degeneration was reduced by an impressive 31 %.
These results are of importance to the ageing population and the elderly. A high dietary intake of the four nutrients is important in the risk reduction of age related eye diseases like AMD.
Reference: JAMA. 2005; 294:3101-3107; Vol. 294, No. 24, December 28, 2005
Last edited December 6, 2012