This article is regarding what to do about hot flashes in menopause. It is important to realize that 80% of women who transition to menopause develop hot flashes and night sweats. Notably, this happens between 45 years and 55 years for most women. Another key point, two methods to fight menopause are non-hormonal methods including a new FDA approved drug and estrogen/progesterone therapy to replace missing hormones. Below I am reviewing both methods.
Non-hormonal methods to fight hot flashes
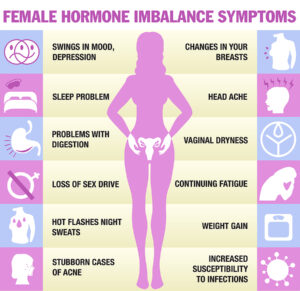
June 7, 2023 CNN published a review article about non-hormonal methods to fight hot flashes. In the article health professionals pointed out that there are a number of steps that the menopausal woman can take to lower the number and intensity of hot flashes. Indeed, menopausal symptoms include not only hot flashes, but also chills, night sweats, sleep problems, mood changes, vaginal dryness and pain during sex. It is important to realize that some women are not good candidates for hormone therapy, because they have a family history of estrogen-dependent cancers, cardiovascular disease, stroke, blood clotting disorders, deep vein thrombosis and chronic liver disease. The North American Menopausal Society just published the 2023 update to their recommendations for non-hormone therapy of menopause.
A new drug blocking hot flashes and night sweats
In this recommendation a new FDA approved drug is included. The pharmacological name is fezolinetant, the brand name is Veozah. To point out, this drug targets the neural activity in the brain that causes hot flashes and night sweats. It binds to the NK3 receptor, which regulates body temperature. The end result is a block of the KNDy (pronounced “candy”) neurons in the brain. To emphasize, these consist of kisspeptin, neurokinin B and dynorphin. The initials led to the abbreviation of the KNDy neurons (pronounced “candy”). To explain, the most common side effects are nausea and headaches. The only other medications that the FDA recognizes as effective for hot flushes and night sweats are low dose SSRI antidepressants.
Other recommendations of the 2023 non-hormone therapy of menopause update
By all means, triggers like caffeine and alcohol overconsumption and smoking should be avoided. Weight loss and cognitive therapy are reducing hot flashes. Clinical hypnosis is also effective as a treatment, as is Gabapentin. Specifically, a low-fat, plant-based diet and a half-cup of cooked soybeans per day led to a 88% reduction in moderate to severe vasomotor symptoms (hot flashes). Researchers compare this to a group with no dietary changes over 12 weeks.
Despite all of these measure menopausal women on hormone replacement did feel a lot more improvement.
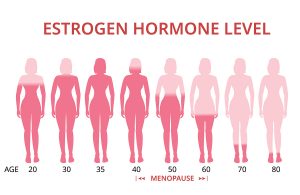
Hormone replacement with estrogen and progesterone
Before we discuss this further a quick review of the Women’s Health Initiative in 2002 is necessary. This was a large study that showed that on Premarin and Progestin, two synthetic hormone products, women came down with breast cancer, heart attacks, stroke, and thromboembolic events. They were using the synthetic drugs conjugated equine estrogen and medroxyprogesterone acetate. The reason these women had to suffer these side effects was because their physicians insisted in using hormones from drug companies rather than compounded bioidentical hormones. But these synthetic hormones were not pure hormones; they were adulterated with side chains. These side chains made the synthetic hormones not fit the body’s hormone receptors. And this is the reason why the synthetic hormones created chaos in form of breast cancer, strokes and heart attacks.
European trials regarding bioidentical hormone treatment
However, studies in Europe showed over many years that hormone replacement with bioidentical estrogen and progesterone creams from compounding pharmacies have no deleterious side effects, but replace the action of the missing hormones in menopause. Women lose their hot flashes and night sweats, regain their previous energy and sleep again through the night. Here is a link what the Mayo Clinic recommends to treat menopause.
Present day recommendation from regenerative physicians
The key about hormone replacement after menopause is to balance estrogen replacement with bioidentical progesterone. The ratio of the two hormones needs to be about 200:1 (or higher) for progesterone versus estrogen. Estradiol, which is the main estrogen in women is a mild carcinogen when not properly balanced with progesterone. By having higher progesterone dosages for hormone replacement, the body is protected from cancer and other side effects. Dr. John Lee years ago coined the term “estrogen dominance”. He also recommended the ratio of 200:1 of progesterone versus estrogen to balance the two hormones. A postmenopausal woman can apply a bioidentical BiEst cream (estrogen) to her skin and combine this with a bioidentical progesterone cream. Alternatively, she may prefer to take oral progesterone (Prometrium) 100 or 200 mg at bedtime. These tablets consist of crystallized bioidentical progesterone. None of this will cause cancer or other detrimental conditions.
Conclusion
Recently a publication describes a new drug that helps with hot flashes. The pharmacological name is fezolinetant, the brand name is Veozah. It blocks special neurons in the brain that are responsible for hot flashes. But possible side effects of this drug are nausea and headaches. Contrary to this there is no side effect with bioidentical hormone replacement when the physician balances the concentration of estrogen and progesterone. In this case the hormone balance prior to menopause simply returns. In this case her hot flashes and other menopausal symptoms simply stop. Anti-aging physicians in Europe have shown decades ago that the described combination of BiEst and Prometrium is safe, contrary to the synthetic drugs that were used in the Women’s Health Initiative where women died from heart attacks, breast cancer and blood clots.