A research group from Boston, MA and New York, NY found that a lack of sleep harms the immune system and causes inflammation. This was summarized in this CNN article.
Specifically, they first conducted experiments with a mouse model. They studied the effects of sleep disruption and sleep deprivation and could later confirm identical changes in man. The observation was that a lack of sleep caused the hematopoietic cells in the bone marrow to proliferate, but the cell diversity was less than in people with normal sleep patterns. The same pattern of bone marrow proliferation was present in mice. This research was published Sept. 21, 2022 in the Journal of Experimental Medicine.
Chronic sleep deficit
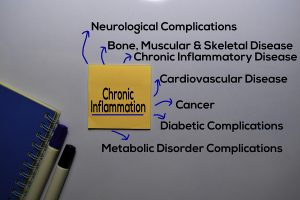
A chronic sleep deficit caused chronic inflammation and eventually autoimmune diseases. Again, this was a pattern present in both the mouse model and in humans. Next the researchers observed what happened with sleep recovery. In the past it was assumed that with sleep recovery all of the physical changes from sleep deprivation would disappear. However, the opposite was true: both in mice and in humans the bone marrow stimulation and the lack of cell diversity persisted.
In the mouse model the researchers could show that there were permanent epigenetic changes, which were caused by sleep deprivation. The same is true with humans, but this is more difficult to show than in the mouse model. The researchers came to the conclusion that sleep deprivation stimulates bone marrow maturation, but restricts the clonal differentiation. In doing so the body initiates inflammation, which becomes chronic even with sleep restoration.
Human sleep studies
There were 14 volunteers that were the test subjects. One group was the normal sleep control. The other group underwent chronic sleep deprivation. Each group did this for 6 weeks. There was a 4-to-6-week washout period. Following this the previous normal sleep group started a 6-week sleep deprivation program. On the other hand, the prior sleep-deprived group switched to 6 weeks of normal sleep. All of the participants had daily late afternoon blood tests.
There are many sleep disruptions, which cause a sleep deficit
In modern life sleep gets disrupted in many ways. There can be sleep fragmentation, sleep restriction, jet lag, obstructive sleep apnea (OSA), and insomnia.
People with these conditions often oscillate between these various types. They may have a few days of normal sleep, but then have sleep deprivation again for a few days. Every time they have sleep deprivation the bone marrow enhances hematopoietic activity. Normally there is a high leukocyte number in the blood at the end of the day and in the morning a lower leukocyte count. But with sleep deprivation there is a high monocyte count in the blood that stays high even when subjects switch back to a normal sleep pattern.
Epigenetic effect of sleep deprivation on bone marrow cells
The authors found that sleep deprivation affects the genetic control of hematopoietic cells in the bone marrow. They called this the epigenetic effect of sleep deprivation. This is responsible for the evening leukocyte response, the monocytosis and the tendency for autoimmune diseases. They summed this up by saying: “Our findings support the hypothesis that periods of poor sleep, even if followed by sleep recovery, have sustained consequences on immunological health.”
Lack of sleep harms the immune system and causes inflammation says the literature
There is ample evidence that a lack of sleep causes cardiovascular disease, diabetes, depression and more frequent infections. Healthy sleep is important when you want to age well without complications. But enough sleep is also necessary to prevent obesity, diabetes and cardiovascular disease. Experts consider getting enough high-quality sleep as essential as a balanced diet and regular exercise.
Conclusion
So far, most researchers believed that when you miss some sleep for a few nights that a afternoon nap or a few nights of longer sleep would compensate for the sleep deficit with no sequelae. Think again, because new research from a group in Boston, MA and New York, NY found that lack of sleep harms the immune system and causes inflammation permanently. Sleep deprivation stimulates the bone marrow cells to multiply and causing proliferation of monocytes, called monocytosis as well. Despite afternoon naps and recovery sleep this condition remains and can lead to autoimmune diseases. All this was unknown up to now. Our bone marrow cells need regular sleep hours to stay diversified and to optimally fight infections in the body. This prevents autoimmune diseases and keeps our defenses against viral diseases strong.