A new disease has arrived, allergies to red meat after a tick bite. This condition has surfaced in Australia and in the southeast of the US. It is linked to the bite by a lone star tick. Researchers determined that alpha-gal, which is galactose-α-1,3-galactose from the saliva of the tick is responsible for causing an allergy. Meat from mammals also contains alpha-gal. Due to a cross reaction between a lone star tick bite and alpha-gal in beef and other meats a person can develop a sensitivity to alpha-gal. This has the name alpha-gal syndrome (AGS). Between 2010 and 2022 the CDC recorded about 110,000 suspected cases of AGS in the US.
Symptoms of alpha-gal syndrome
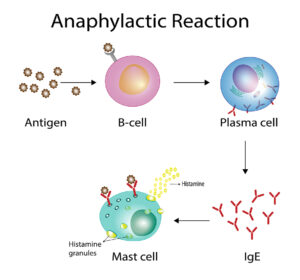
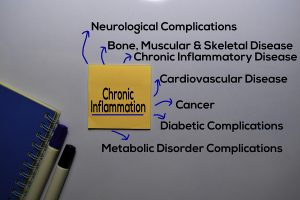
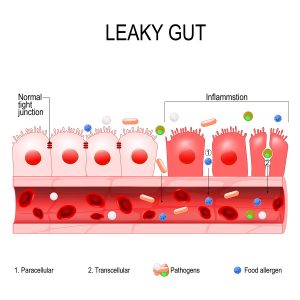
A person who was previously sensitized by a lone star tick bite often only gets symptomatic after eating beef. The symptoms are hives, a skin rash, nausea or vomiting, heartburn or indigestion and diarrhea. Other symptoms could be a cough, shortness of breath, difficulty breathing or a drop in blood pressure. Some patients develop swelling of the lips, throat, tongue, or eye lids. Others complain of dizziness, faintness or severe stomach pains. These symptoms usually develop 2 to 6 hours after eating a meal with beef or dairy products. The person who was previously bitten by a lone star tick was sensitized following this encounter and produced specific antibodies against alpha-gal. The second encounter of the body from ingested alpha-gal containing food is the reason why the allergic reaction takes place. The more alpha-gal is ingested by different foods that contain it, the more severe the allergic reaction becomes.
Diagnostic tests for alpha-gal sensitivity
Allergists have the following tests available to them to check your immune system.
- One test is called the alpha-gal U953 immunocap, a blood test.
- The mammalian meats immunocap (Beef, Lamb, Mutton, Pork and Rabbit are available) shows specific antibodies as a result of exposure to these meats.
- In severe cases of alpha-gal sensitivity blood tests for a mast cell tryptase level may also be necessary. This test can distinguish between a higher or lower risk of alpha-gel sensitivity. Tryptase is an enzyme, which is higher in people with mastocytosis. There is often an elevation of tryptase in patients who have allergies to both insect bites and tick bites.
Foods that contain alpha-gal
The Australasian Society of Clinical Immunology and Allergy describes in great detail what foods contain alpha-gal and what not. The main culprit in developing alpha-gal syndrome is mammalian meat. The most popular among these is beef, but veal, pork, lamb, buffalo, venison, rabbit and guinea pig also belong into this category. Other meats are deli meats like bacon, ham, salami, silverside, chorizo, prosciutto and others. When a person reacts to eating one or more of these items, we are dealing with a cross reaction. It is between the alpha-gal from the original tick bite and alpha-gal from the meat the person ingested.
There are more obscure mammalian meats that contain alpha-gal: whale, dolphin, seal, goat, kangaroo, wallaby and possum. But gelatin products and fats from mammals also contain alpha-gal.
What foods do not contain alpha-gal?
The following foods are OK to eat for people with alpha-gal sensitivity: chicken, mollusks, crustaceans, turkey, quail, goose, fish, duck, eggs, legumes, lentils and soy products (tofu, tempeh). According to the allergy.org website, you have to be careful about jams, soups and gravies, as merchants often mix gelatines into their products. Stay away from energy drinks with taurine, sausages (even chicken sausage) and cheese spread. Avoid rennet, jelly-based lollies, mousses and desserts. All of them contain alpha-gal.
Treatment for alpha-gal syndrome
There is no known treatment for sensitivity to alpha-gal. However, experience has taught allergists that strict avoidance of alpha-gal in food improves the symptoms. After about 3 to 4 years of a strict diet that excludes alpha-gal many patients are no longer sensitive to alpha-gal and can tolerate a certain amount of alpha-gal in their diet. But others continue to be sensitive to alpha-gal. They have to adhere to strict avoidance of alpha-gal in food and stay away from tick bites.
Conclusion
A new condition, alpha-gal syndrome has joined the rare, but important group of new diseases. It is a sensitivity to a sugar, called galactose-α-1,3-galactose, or alpha-gal. It is present in the mouth and saliva of the lone-star tick in the US and Australia. A bite from this tick can be the first sensitizer in a human. But unfortunately, alpha-gal is also present in many foods as mentioned in detail above. Repeated exposure to alpha-gal regardless of the origin causes hypersensitivity, which can get life-threatening. There is no treatment for this condition other than to adopt a very meticulous avoidance of alpha-gal in the diet. After 3 to 4 years of such a diet the hypersensitivity to alpha-gel disappears in many, but not in all patients. When the hypersensitivity persists, the patient has to continue with the alpha-gal avoidance diet.