This book entitled “Healing Gone Wrong – Healing Done Right” (Amazon, March 18, 2016) is dealing with the practice of medicine then and now. Medical errors, false diagnoses and wrong treatments are nothing new in the history of medicine. It happened in the past, and it is happening now. My first book was about anti-aging. The title was “A Survivor’s Guide to Successful Aging” (Amazon 2014).
Book overview
Chapter 1
Here I describe describe that famous people like President Kennedy, Elvis Presley, Churchill, Beethoven or more recently Michael Jackson have something in common: all of them suffered the consequences of blatant medical mistakes. In Beethoven’s time lead containing salves to plug the drainage holes from removing fluid from his abdomen caused lead poisoning. In this chapter I review also how doctors treated the illnesses of the above-mentioned celebrities, but then ask the question: “What better treatments have offered to prevent some of the disastrous treatment outcomes?”
Chapter 2
Modern drugs seem to come and go. We learn that twenty-first century medications that are supposed to be the latest therapeutic agents are having their potentially deadly consequences too: COX-2 inhibitors, the second generation arthritis drugs cause strokes and heart attacks! Your doctor may still prescribe some of these dangerous drugs for arthritis now.
Chapter 3
This chapter deals with the fact that medical treatments for people’s diseases may be inappropriate when the doctor treats only symptoms, but the doctor does nothing about the causes of their illnesses. This is a scary thought.
Chapter 4
What does it take to prevent these poor health outcomes, so that we will be able to prevent any disastrous outcomes pertaining to our own health care in the present and future? As we will see, the problem today is still the same as it was in the past, namely that many physicians still like to treat symptoms instead of the underlying cause of an illness. Big Pharma has the seducing concept of a pill for every ill, but it is not always in your best interest, when these medications have a slew of side effects. “Gastric reflux” means a mouthful of stomach acid. Big Pharma simply offers the patient with the symptom of gastric reflux a multitude of medications to suppress this symptom. But it is more important to dig deeper to find the reason for the illness and treat the underlying cause.
Chapter 5
We all need our brain to function. This chapter concentrates on the brain and how we can keep our brains functioning optimally until a ripe old age. This review spans from prevention of head concussions to avoiding type 3 diabetes (insulin sensitivity from overconsumption of sugar). It manifests itself in Alzheimer’s disease. It is a form of diabetes of the brain that leads to deposits of a gooey substance. Prevention of this condition is also reviewed .
Chapter 6
This chapter reviews what we now know about how to keep a healthy heart. Certain ingredients are necessary such as regular exercise, a healthy Mediterranean diet, supplements etc. The good part is that what is good for the heart is also good for the brain. You are preventing two problems (brain and heart disease) at the same time.
Chapter 7
What should we eat? And why does healthy food intake matter? Without the right ingredients of our body fuel, the body machinery will not work properly. The Mediterranean diet is an anti-inflammatory diet that is particularly useful.
Chapter 8
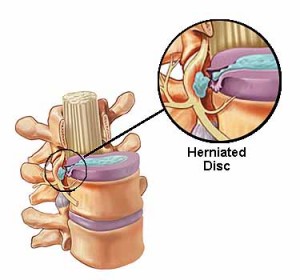
We need healthy limbs, bones and joints. We are meant to stay active in our eighties and nineties and beyond. No osteoporosis, no joint replacements, no balance problems that result in falls! Learn about how to deal with problems like these in this chapter.
Chapter 9
This chapter deals with detoxification. What do we do as we are confronted with pollution, with radiation in the environment and poisons in our daily food? A combination of organic foods, intravenous chelation treatments and taking supplements can help us in that regard.
Chapter 10
I am dealing here about reducing the impact of cancer in our lives. A lot of facts have come out in the past 10 years telling us that reduction of sugar and starchy food intake reduces cancer. Curcumin, resveratrol and vitamin D3 supplements also reduce cancer rates as does exercise and stress management. All of this is reviewed here.
Chapter 11
This chapter tells you all you need to know about your hormone status. Women need to avoid estrogen dominance; both sexes need to replace the hormones that are missing. By paying attention to your hormonal status and replacing the missing natural hormones with bioidentical ones, most people can add 10 to 15 years of useful, active life!
Chapter 12
Here you will learn more about anti-aging. You will learn about the importance to keep your mitochondrial DNA healthy. Apart from that there are ways how to keep your telomeres longer; certain supplements that are reviewed will help. Also your lifestyle does make a big difference in how old you can turn.
Chapter 13
This chapter investigates the limits of supplements. Many supplements are useful, but you do not want to overdo it and get into toxic levels. More is not necessarily better!
Chapter 14
Here is a review of an alternative approach to treating ADHD. Attention deficit and hyperactivity disorder has been over diagnosed, has been neglected and has been over treated with dangerous drugs. An alternative treatment plan is discussed, which includes a combination of therapeutic steps.
Chapter 15
This gives you a brief summary of the book.
Kirkus Review
Kirkus Reviews reviewed the book on March 17, 2016: “A retired physician details how various preventative measures can fend off disease and disability in this consumer health guide. Schilling (A Survivor’s Guide to Successful Aging, 2014) had a family medicine practice in Canada for many years before retiring. Although Schilling ventures into some controversial territory in his latest book, it’s generally an engaging, helpful synthesis of ideas that draws on reputable research from the Mayo Clinic and other sources. Overall, it serves as an intensely detailed wake-up call to the importance of preventative health. He largely brings an accessible and even-tempered tone to his narrative, warning readers, for example, that preventative health measures can only aid in “a delay of aging, not ‘eternal living.’ ” A thought-provoking, impassioned plea to be proactive about one’s health.”
Conclusion
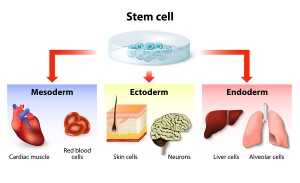
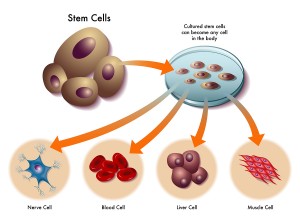
In this book it becomes evident that it is better to prevent an illness whenever possible rather than to wait for illness to set in and cause disabilities or death. You heard this before: “Prevention is better than a cure” or “an ounce of prevention is better than a pound of cure”. I will give an explanation, based on scientific data that there is indeed evidence to support these notions on a cellular level.
Mitochondria, the energy packages within our cells
The mitochondria, the energy packages within our cells, are the driving force that keep people vibrantly healthy well into their nineties. All this can only happen when the mitochondria function properly. If toxins poison the mitochondria and as a result they malfunction, we are not looking at a person with vibrant health. Instead sixty or seventy year-olds may use a wheelchair. If you want a life without disabilities, a life without major illnesses and enjoy good health to a ripe old age, you are reading the right book.
The book is written in American English.
Available in the US: http://www.amazon.com/gp/product/1523700904
In Canada: https://www.amazon.ca/Healing-Gone-Wrong-Done-Right/dp/1523700904/
In other countries the book is available through the local Amazon websites.