Much has been written about what happens when women get into menopause. This begs the question: do men experience a change of life? As a matter of fact, they do. It is called “andropause”, and they can experience problems as a result. Here is a study from the Massachusetts General Hospital in Boston, MA, which was published in the New England Journal of Medicine (Sept. 2013) describing in detail what happens when men get into andropause (the male equivalent of the menopause).
We know from other studies that in obese men testosterone is converted into estrogen because of the enzyme aromatase that converts testosterone into estrogen resulting in erectile dysfunction and loss of sex drive. In lean men above the age of 55 there is a true testosterone reduction because the testicles produce less testosterone. This results in less sex drive, moodiness and lack of energy. But these men will do well with bioidentical testosterone replacement.
Main findings of the Massachusetts General Hospital study:
- Testosterone was responsible for thigh muscle development and leg press strength, for erectile function and sexual desire.
- Surprisingly, estradiol (the main estrogen component in both sexes) plays a significant part in sexual desire in the male. This became particularly apparent in the post-andropause male who desired hormone replacement. When bioidentical testosterone is used to replace what’s missing there was no problem with sexual desire or erectile function as a small amount of the testosterone was aromatized into estradiol. The researchers were able to measure both testosterone and estradiol levels.
- Here is a surprising fact: a lack of estrogen leads to abdominal obesity. This could also be verified by hormone measurements.
- In the past doctors used synthetic testosterone products like methyltestosterone, danazol, oxandrolone, testosterone propionate, testosterone cypionate or testosterone enanthate. The problem with these synthetic testosterone products is that the body cannot metabolize a portion of them into estrogen that is desirable for a normal sex drive, so the testosterone compounds alone are not doing their job as well as the bioidentical testosterone that the body can aromatize.
In obese men the problem is that there is too much estrogen in the system, which leads to a disbalance of the hormones in the male with a relative lack of testosterone. Overweight and obese men produce significant amounts of estrogen through aromatase located in the fatty tissue. Aromatase converts testosterone and other male type hormones, called androgens, into estrogen. Excessive levels of estrogen cause breast growth, muscle weakness, lead to abdominal fat accumulation, heart disease and strokes. Dr. Lee described what happens in men who enter andropause years ago as indicated under this link.
Testosterone to estrogen ratio:
Dr. Lee indicated that in his opinion saliva hormone testing is more reliable than blood tests (Ref. 1). One of the advantages of doing saliva hormone tests of estrogen and testosterone is that you can calculate directly the ratios of these two hormones. In hormonally normal younger males the testosterone to estrogen ratio is larger than 20 – 40 (Ref.2). The testosterone to estrogen ratio in obese men is typically less than 20 meaning it is too low. But lean men in andropause produce too little testosterone and their testosterone to estrogen ratio is also less than 20, because they may still have enough estrogen in their system from aromatase in the fatty tissue, but they are lacking testosterone due to a lack of its production in the testicles (Ref. 1 and 2).
When a man in andropause is given bioidentical hormone replacement with a testosterone gel or bioidentical testosterone cream this is absorbed into the blood and body tissues and then partially metabolized into a small amount of estrogen. This can be seen when saliva hormone tests are done; a higher level of testosterone is detected and much lower estrogen level so that the testosterone to estrogen ratio is now 20 to 40 or higher and the affected person will no longer be the “grumpy old man” that had been a source of distress to his partner before.
This New England Journal of Medicine study is important because it confirmed what anti-aging physicians had been saying for years: a small amount of estrogen is necessary for the male for bone health as estrogen receptors will regulate the bone density, it also helps for a normal sex drive. The same is true for women: a small amount of the opposite hormone (testosterone) will help a woman’s sex drive, but she needs the right mix of progesterone to estrogen (a progesterone to estrogen ratio of 200:1 using saliva tests) to feel perfectly normal as a women.
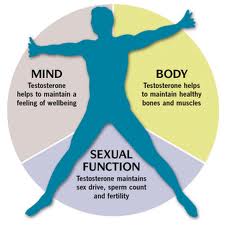
Health and well-being of a man depend on normal testosterone levels:
It is important to realize that testosterone is not only supporting a man’s sex drive and libido, key organs like the heart, the brain and blood vessels contain testosterone receptors as well. The body of a man was designed to respond to testosterone all along. It is when testosterone production is no longer keeping up that premature aging becomes apparent, as the target organs do no longer receive the proper signals.
A healthy heart in a man depends on regular exercise and testosterone stimulation whether he is young, middle aged or old. The same is true for the lining of the arteries where testosterone receptors are present to help with the normal adjustment to exercise and relaxation. The brain cells have receptors for all of the sex hormones and in a man they are used to higher levels of testosterone and lower levels of progesterone and estrogen. If you take the balance away, the aging man will feel miserable and grumpy. Depression will set in. Here is a brief review how one man’s life has been changed by testosterone replacement.
So, bioidentical hormone replacement is not just a matter of replacing one hormone, you need to pay attention to all of the hormones. Lifestyle issues enter the equation as well. I have reviewed the issue of bioidentical hormone replacement for women and men in this blog.
Conclusion:
When a man reaches the age of 55 or older there comes a point where a lack of testosterone and estrogen sets in. It is wise to start doing intermittent blood or saliva hormone tests before this point is reached in order to gage when bioidentical hormone replacement treatment should be given. Along with an assessment regarding the hormone status it would be wise to also assess lifestyle issues as often other factors play a role in premature aging. I have reviewed these factors systematically in a recent publication (Ref. 3). It is best to combine bioidentical hormone replacement with life style interventions to achieve optimal preservation of a man’s health.
More information about male menopause (=andropause): http://nethealthbook.com/hormones/hypogonadism/secondary-hypogonadism/male-menopause/
References:
- John R. Lee, MD: “Hormone Balance for men- what your doctor may not tell you about prostate health and natural hormone supplementation”. 2003 by Hormones Etc.
- George Gillson, MD, PhD, Tracy Marsden, BSc Pharm: “You’ve Hit Menopause. Now What?” 2004 Rocky Mountain Analytical Corp. Chapter 9: Male Hormone Balance (p.118-148).
- Dr.Schilling’s book, March 2014, Amazon.com:“A Survivor’s Guide To Successful Aging: With recipes for 1 week provided by Christina Schilling”.
Last edited Nov. 8, 2014