When a person has osteoarthritis, steroid injections are doing harm, but stem cells help. A new study published in the journal “Radiology” came to the conclusion that steroid injections are doing harm.
The article was published on October 15, 2019. 459 patients with osteoarthritis of knees or hips received injections with intraarticular corticosteroids or placebo to conduct this study. As a matter of fact steroid injections are a standard treatment for moderate to severe osteoarthritis. The injections consisted of triamcinolone 40 mg mixed with a local anesthetic. 36 of these patients (8%) had adverse events in their joints.
Here is the break down of these negative events following intraarticular corticosteroid injections.
- Accelerated osteoarthritis progression (6%)
- Subchondral insufficiency fracture (0.9%)
- Osteonecrosis (0.7%)
- Rapid joint destruction with bone loss (0.7%)
Critical analysis of effects of intraarticular corticosteroid injections
The authors reviewed the literature and came across an evidence-based review by the Cochrane Musculoskeletal Group involving 1767 participants. The review showed an overall low evidence for all outcomes. Intraarticular corticosteroid injections were inconsistent and variations between trials were high. Certainly, there was a moderate improvement of joint pain, and physical joint function improved as well.
But then again more severe osteoarthritis in knee or hip joints showed a lack of improvement and in many cases even joint deterioration. With this in mind, these cases often ended up with total hip or total knee replacements. Overall the Cochrane review showed a lack of objective evidence of symptom improvement after intraarticular corticosteroid injections in people with osteoarthritis.
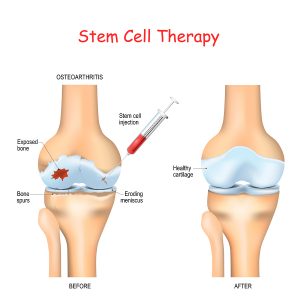
Mesenchymal stem cell injections for osteoarthritis
A fairly recent alternative approach to treating osteoarthritis is by mesenchymal stem cell injection with platelet-rich plasma activation. Researchers conducted a meta-analysis of 35 studies regarding knee osteoarthritis and mesenchymal stem cell injections in 2018. There were minor adverse events like knee pain and swelling. No serious side effects of the stem cell treatments were noted. The outcome of the treatment was classified as “very low” to “low”. The reason for this were poor study designs, large heterogeneity among the studies and wide variation among the 95% confidence intervals regarding study outcomes.
Australian study of mesenchymal stem cell injections into symptomatic knees
A short-term study from Australia examined 30 patients with mesenchymal stem cell therapy for knee osteoarthritis. There were two treatment groups. One group received 100 million adipose tissue derived mesenchymal stem cells into symptomatic osteoarthritis knee joints. Another treatment group received 100 million mesenchymal stem cells twice, namely at baseline and at 6 months after the first injection. The third group served as a control with continued conservative management. All of the groups had baseline MRI scans (magnetic resonance imaging) to assess the knee conditions. Both treatment groups had pain and inflammation at baseline. After 1 year following the initial treatment the patients had repeat MRI scans. They showed modification of the disease process in the treatment arm, while the controls had deteriorating osteoarthritis. The researchers concluded that adipose derived mesenchymal stem cell treatment of knee osteoarthritis has the potential of preventing disease progression.
Why stem cells help with osteoarthritis of the knees and the hips
Here is a research project between researchers from Palm Harbor, Florida and researchers from Serbia. The Center for Molecular Medicine and Stem Cell Research, Faculty of Medical Sciences University of Kragujevac, Serbia reviewed the literature on treatment of osteoarthritis.
The researchers explain that the physician can easily harvest mesenchymal stem cells by doing a liposuction of fat cells. These stem cells maintain their differentiation potential and there is only minor immunological rejection because of low histocompatibility antigen expression. As a result mesenchymal stem cells stay in the joint where they are injected.
Two processes that occur with injected stem cells
Two main advantages of mesenchymal stem cells stand out. Mesenchymal stem cells are capable of building up hyaline cartilage and in addition they have immunosuppressive characteristics. In comparison with controls patients who receive intraarticular injections of mesenteric stem cells have less pain and less swelling.
This review paper cites all the major animal and human studies regarding mesenchymal stem cell therapy for osteoarthritis. It concludes that stem cell therapy is most effective in mild to moderate osteoarthritis cases. It stresses the point that stem cells can regenerate joint tissues and that the inflammatory process of osteoarthritis is interrupted by the stem cells. This stabilized the osteoarthritic condition.
Conclusion
Mesenchymal stem cells derived from fatty tissue will repair tissue defects in joints afflicted by osteoarthritis. The stem cells also take care of the inflammation, which takes care of pain and swelling. Range of motion of the joint increases following stem cell treatment. Other studies have shown that intraarticular steroid injections do not interrupt the degenerative process. MRI scan studies have shown deterioration of the joint tissues following steroid injections. All in all, stem cell treatments of joints with osteoarthritis are superior to a treatment with steroid injections.