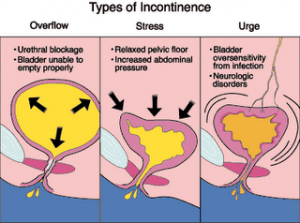
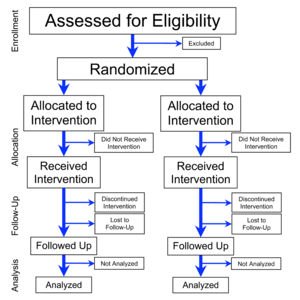
Once hailed as the miracle pill for the aging woman, hormone replacement therapy (HRT) is now being approached with caution. The infamous Women’s Health Initiative study, which first disproved benefits of hormone therapy, first pointed out an increase of breast cancer risk and risk of cardiovascular disease. On re-analysis of the data the Journal of the American Medical Association has published a study in its issue of February 23, 2005, which shows some more reason for caution with HRT. The previous notion that hormone replacement would improve the symptoms of urinary incontinence has turned out to be a fallacy. Dr. Susan Hendrix and her colleagues from Wayne State Untiversity School of Michigan in Detroit analyzed the data from 23,296 women with urinary incontinence. In randomized trials they received either estrogen alone, estrogen with progestin (Prempro) or the placebo effect (“fake pills”). Among those who were continent at the baseline, both, estrogens alone as well as the combination therapy were associated with an increased risk of incontinence at one year. Estrogen (Premarine) alone produced the most marked effect: stress incontinence increased by a factor of 2.15, the combination therapy increase stress incontinence by a factor of 1.87. In addition, women who were already suffering of incontinence, tended to report a worsening of their symptoms after beginning hormone therapy. The Women’s Health Initiative trials were stopped because the treatment risks appeared to outweigh its benefits. These new findings tilt the scales even further against hormone therapy, the authors say in their study.
Reference: National Review of Medicine, Canada, March 15, 2005, page 28
Comments on Nov. 8, 2012: We have to keep these observations in perspective. The authors of that study were using the “regular” Big Pharma manufactured hormone substitutes that the body cannot read. There are no Premarin or Provera receptors in the tissue, only testosterone receptors, estrogen receptors and progesterone receptors. These artificial hormones cannot be metabolized in the woman’s body into testosterone as bio-identical estrogen and progesterone would, because they are structurally different from the bio-identical hormones. The sad truth is that an anti-aging physician could have treated these poor women with incontinence safely by prescribing small amounts of testosterone cream that would have had to be applied to the urethral opening. From there the body would have sent it to the bladder, the bladder sphincter and the testosterone receptors that control these tissues and would have taken care of the incontinence problem. You do not need a clinical trial. This type of treatment has been used in Europe for decades and has been used in the US for maybe 10 to 15 years as well by some open minded urologists and anti-aging physicians. The heading for this post is only applicable for HRT in the conventional sense (using Big Pharma drugs), but none of this applies to bio-identical hormone replacement for menopause.
More info on bio-identical hormone replacement in menopause: http://nethealthbook.com/hormones/hypogonadism/secondary-hypogonadism/menopause/
Last edited October 28, 2014