Sleeping problems (insomnia) are very common. About 10% of the population suffers from chronic insomnia; 30% of the population suffers from occasional sleep problems. In a large outpatient population of a clinic consisting of 3500 patients who had at least one major clinical condition, 50% complained of insomnia, 16% had severe symptoms, 34% had mild symptoms (Ref.1). Insomnia is more common among women, and older people as well as in people with medical or psychiatric illnesses. Long-term studies have shown that the same insomnia problems persist throughout many years. It is not possible to offer a simple remedy for insomnia, because insomnia is a complex problem. Here I will discuss some of the causes of insomnia and also discuss some of the treatment options.
Symptoms of insomnia
The person who suffers from insomnia will usually state that they have problems falling asleep. Worries of the day suddenly circulate through their thoughts and they toss and turn nervously looking at the clock from time to time and getting more and more anxious that they cannot sleep. Others fall asleep OK, but in the middle of the night they wake up perhaps to visit the restroom, but then they cannot go back to sleep. Others wake up 2 hours before their normal alarm clock time and they feel their stomach rumbling making it impossible to fall back to sleep. Older people with chronic diseases and general poor health suffer more from insomnia. In this setting insomnia may be more related to the underlying disease rather than old age. Psychiatric disorders also are associated with more insomnia. Treat the underlying psychiatric illness, and the insomnia disappears.
Although insomnia is a sleep disturbance during the nighttime, people who are affected with this complain of daytime fatigue, of overstimulation, yet they catch themselves making frequent mistakes, and their inability to pay attention gets them involved in accidents and falls. Longitudinal studies have shown (Ref. 1) that people with chronic insomnia are more likely to develop psychiatric disease, such as major depression, anxiety disorder and alcohol and substance abuse. Unfortunately these disorders can by themselves again cause insomnia, which reinforces chronic insomnia. Insomnia leads to poorer social and physical functioning, affects emotions, leads to a lack of vitality and physical endurance, contributes to worsening of pain and can affect general and mental health.
Research about insomnia
Much has been learnt from sleep studies using polysomnography monitoring during a full night’s sleep. These studies have been used mainly as a research tool. In such studies eye movements, brain wave activity, muscle activity, chest movements, airflow, heart beats, oxygen saturation and snoring (with a microphone) are all simultaneously recorded. This way restless leg syndrome, sleep apnea, snoring, seizure disorders, deep depression etc. that can all lead to insomnia can be diagnosed and separated from insomnia. The stages of sleep (wakefulness, stage 1 to 3 sleep and the REM sleep stage) can also be readily measured using polysomnography (Ref.2). According to this reference the majority of insomnia cases do not need this complex procedure done.
Causes of insomnia
Traditionally insomnia cases are classified into primary insomnia and secondary insomnia. Secondary insomnia is caused by all of the factors discussed below. When they are dealt with, we are left with cases of primary insomnia.
The following medical conditions can cause insomnia: heart disease, pulmonary diseases like asthma and chronic obstructive pulmonary disease (COPD); gastrointestinal disease like liver cirrhosis, pancreatitis, irritable bowel syndrome, ulcers, colitis, Crohn’s disease; chronic kidney disease; musculoskeletal disease like arthritis, fractures, osteoporosis; neurodegenerative disease like MS, Parkinson’s disease, Alzheimer’s disease; endocrine disease like diabetes, hyper- or hypothyroidism, adrenal gland fatigue and insufficiency; and chronic pain conditions. Also, psychiatric conditions like major depression, schizophrenia and anxiety disorders can cause insomnia.
This list in not complete, but it gives you an idea of how complex the topic of insomnia is.
The physician who is seeing a patient with insomnia needs to rule out any of these other causes of insomnia to be certain that the only condition that is left to treat in the patient is insomnia itself. The other diagnoses have to be dealt with separately or else treatment of insomnia will fail.
Ref. 1 points to a useful model of how to think about causation of insomnia: there are three points to consider, namely predisposing, precipitating, and perpetuating factors. Let’s briefly discuss some of these.
Predisposing factors
We are all different in our personal make-up. If you are well grounded, chances are you are not susceptible to insomnia. Anxious persons or persons who have been through a lot of negative experiences in life will have personality traits that make them more prone to insomnia. Lifestyle choices such as late nights out, drinking with the buddies in a bar (extreme circadian phase tendencies) will have an impact on whether or not you develop insomnia.
Precipitating factors
A situational crisis like a job change or the death of a loved one can initiate insomnia. However, there could be a medical illness such as a heart attack, a stroke or the new diagnosis of a psychiatric illness that has become a precipitating factor. Sleep apnea and restless leg syndrome belong into this group as well as would the stimulating effect of coffee and caffeine containing drinks. Jet lag and nighttime shift work can also be precipitating factors.
Perpetuating factors
Daytime napping to make up for lost sleep the night before can undermine sleep initiation the following night, which can lead to a vicious cycle. Similarly, the use of bedtime alcoholic drinks leads to sleep disruption later that night and can become a perpetuating factor, if this habit is maintained. Even the psychological conditioning of being anxious about whether or not you will fall asleep easily or not the next night can become a perpetuating factor.
I will return to this classification and the factor model of causation of insomnia when we address treatment options.
Drugs that can cause insomnia
One major possible cause for insomnia can be side effects from medications that patients are on (would belong to the ‘perpetuating factors’ among causes). Physicians call this “iatrogenic insomnia”. The antidepressants, called selective serotonin reuptake inhibitors (SSRI’s) like Prozac are particularly troublesome with regard to causing insomnia as a side effect. Other antidepressants like trazodone (Desyrel) are used in small doses to help patients with insomnia to fall asleep. Some asthmatics and people with autoimmune diseases may be on prednisone, a corticosteroid drug. This can cause insomnia, particularly in higher doses; so can decongestants you may use for allergies; beta-blockers used for heart disease and hypertension treatment; theophylline, an asthma medication and diuretics. Central nervous stimulants like caffeine or illicit drugs can also cause insomnia. Hormone disbalance in general and hyperthyroidism specifically as well as Cushing’s disease, where cortisol levels are high will cause insomnia.
Treatment of insomnia
So, how should the physician approach a patient with insomnia? First it has to be established whether there is secondary insomnia present due to one of the predisposing, precipitating or perpetuating factors. In other words, is there secondary insomnia due to other underlying illnesses? If so, these are being addressed first. Lifestyle choices (staying up late every night) would have to be changed; alcohol and drug abuse and overindulging in coffee or caffeine containing drinks needs to be dealt with. Cognitive therapy may be beneficial when mild depression or anxiety is a contributing factor to insomnia.
The remaining insomnia (also medically termed “primary insomnia”) is now being treated.
The following general points are useful to get into the sleeping mode (modified from Ref. 3):
- Ensure your bedroom is dark, soundproof, and comfortable with the room temperature being not too warm, and you develop a “sleep hygiene”. This means you get to sleep around the same time each night, have some down time 1 hour or so before going to bed and get up after your average fill of sleep (for most people between 7 to 9 hours). Do not sleep in, but use an alarm clock to help you get into your sleep routine.
- Avoid caffeine drinks, alcohol, nicotine and recreational drugs. If you must smoke, don’t smoke later than 7PM.
- Get into a regular exercise program, either at home or at a gym.
- Avoid a heavy meal late at night. A light snack including some warm milk would be OK.
- Do not use your bedroom as an office, reading place or media center. This would condition you to be awake. Reserve your bedroom use only for intimacy and sleeping.
- If you wake up at night and you are wide awake, leave the bedroom and sit in the living room doing something until you feel tired and then return to bed.
- A self-hypnosis recording is a useful adjunct to a sleep routine. Listen to it when you go to bed to give you something to focus on (low volume) and you will find it easier to stop thinking.
Drugs and supplements for insomnia
1. In the past benzodiazepines, such as diazepam (Valium), lorazepam (Ativan), fluorazepam (Dalmane), temazepam (Restoril), triazolam (Halcion) and others were and still are used as sleeping pills. However, it was noted that there are significant side effects with this group of drugs. Notably, there is amnesia (memory loss), which can be quite distressing to people such as not remembering that someone phoned while under the influence of the drug, you promised certain things, but you cannot remember the following morning what it was. Another problem is the development of addiction to the drugs with worse insomnia when the drugs are discontinued. Many physicians have stopped prescribing benzodiazepines.
2. There are non-benzodiazepines drugs that are used as sleeping pills (hypnotics), such as Zaleplon (Sonata), Zolpidem (Ambien) and Eszopiclone (Lunesta). They seem to be better tolerated.
3. Ramelteon, a melatonin agonist, is available by prescription in the US. It probably is the best-tolerated mild sleeping pill and works similar to melatonin, but is more expensive. Chances are that your physician likely would prescribe one of the non-benzodiazepines drugs or Ramelteon for you as they do not seem to be addicting.
4. However, there is an alternative: Many patients with insomnia tolerate a low dose of trazodone (Desyrel), which is an antidepressant with sleep restoring properties. A low dose of 25 to 50 mg at bedtime is usually enough for insomnia. This allows the patient to fall asleep within about 30 minutes of taking it, and sleep lasts through most of the night without a hangover in the morning. Many specialists who run sleep laboratories recommend trazodone when primary insomnia is diagnosed. However, this is still a drug with potential side effects as mentioned in the trazodone link, but 50 mg is only ¼ of the full dose, so the side effects will also be less or negligible.
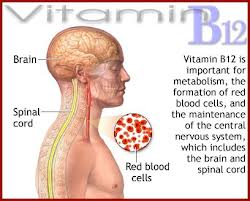
5. I prefer the use of melatonin, which is the natural brain hormone designed to put us to sleep. Between 1 mg and 6 mg are sufficient for most people. We know from other literature that up to 20 mg of melatonin has been used in humans as an immune stimulant in patients with metastatic melanoma with no untoward side effects other than nightmares and some tiredness in the morning. A review from the Vanderbilt University, Holland found melatonin to be very safe as a sleeping aid. There are several melatonin receptors in the body of vertebrates (including humans), which are stimulated by melatonin.
6. Other natural methods are the use of L-Tryptophan at a dose of 500 mg at bedtime, which can be combined with melatonin. It is the amino acid contained in turkey meat, which makes you tired after a Thanksgiving meal. GABA is another supplement, which is the relaxing hormone of your brain, but with this supplement tolerance develops after about 4 to 5 days, so it is only suitable for very short term use. Herbal sleep aids are hops, valerian extract and passionflower extract. They are available in health food stores.
Conclusion
A lack of sleep (insomnia) is almost a given in our fast paced lives.
When it comes to treatment, all of the other causes of secondary insomnia need to be treated or else treatment attempts would fail. What is left is primary insomnia. This is treated as follows:
We need to review our sleeping habits, lifestyles and substance abuse. Remove what is detrimental to your sleep. Start with the least invasive treatment modalities such as self-hypnosis tapes, melatonin, L-Tryptophan or herbal extracts. Should this not quite do the trick, asks your doctor for advice. The non-benzodiazepines drugs or Ramelteon would be the next level up. It may be that an alternative such as low dose trazodone would be of help. Only, if all this fails would I recommend to go to the more potent sleeping pills (keep in mind the potential for addiction to them).
References
1. David N. Neubauer, MD (John Hopkins University, Baltimore, MD): Insomnia. Primary Care: Clinics in Office Practice – Volume 32, Issue 2 (June 2005) © 2005, W. B. Saunders Company
2: Behrouz Jafari, MD and Vahid Mohsenin, MD (Yale Center for Sleep Medicine, Yale University School of Medicine, New Haven, CT, USA): Polysomnography. Clinics in Chest Medicine – Volume 31, Issue 2 (June 2010), © 2010 W. B. Saunders Company
3. Jean Gray, editor: “Therapeutic choices”, 5th edition, Chapter 8 by Jonathan A.E. Fleming, MB, FRCPC: Insomnia, © 2008, Canadian Pharmacists Association.
Last edited Sept. 28, 2014