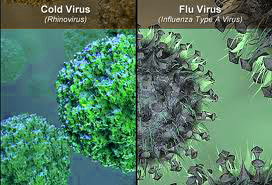
Every year there is concern about the upcoming flu season. Mostly the discussion centers on the composition of the latest flu bugs and what type of strains would be included in the latest vaccine recommended. The first flu case of the season has just been reported in a child. Here I am going to review what you can do to minimize your probability of getting the flu, or if you get it, how to minimize the severity of the illness.
The immune system
We know for some time that the antibody-mediated immune system is what helps overcome flus. The body’s immune system produces antibodies against the flu via T-helper cells that recognize the glycoprotein (hemagglutinin) of the flu virus and pass a signal on to B cells (bone marrow derived lymphocytes), which in turn are turned on to produce a lot of antibodies (Ref.1). These protect you from future flus of this type. If you have pre-existing antibodies that fit the bug in circulation you are OK ,and you will usually not get the disease.
The factors that protect you from the flu
However, there are many other factors that support your immune system. I will discuss the most important factors in more detail here.
1. We do know that vitamin D3 strengthens the immune system. I would recommend 1000 to 2000 IU per day in the wintertime, but up to 4000 IU or 5000 IU per day during an active epidemic would be reasonable. There is less flu when people are taking Vitamin D3 supplements.
Influenza A was reduced in school children supplemented with 1200IU of vitamin D3. This study recommended higher doses of 2000 to 7000 IU of vitamin D3 per day; but it also stated that as a precaution serum vitamin D levels should be monitored (technically it is serum 25-hydroxy-vitamin D levels that are measured) to avoid vitamin D toxicity. Normal levels are between 40-70 nanograms per ml. Toxic levels are above 100 nanograms per ml. Your family doctor can order a serum 25-hydroxy-vitamin D level for you.
2. Eating fruit and vegetables is important for maintaining a healthy immune system. In a randomized study from Belfast, UK elderly volunteers (82 of them, aged 65 to 85) were assigned to either eat 2 portions or 5 portions of fruit and vegetables per day over 16 weeks. At 12 weeks into the trial both groups received a Pneumovax II vaccination, and the antibody response was measured at the end of the 16th week of the study. There was a significant increase in antibody binding capacity to pneumococcal capsular polysaccharide in the 5 portion fruit and vegetable group compared to the 2 portion group that had no such increase. The authors concluded that there is a measurable improvement of the immune system when an older population increases their fruit and vegetable intake.
3. Avoid stress, because stress has been shown to weaken the immune system. This review shows that the immune system is weakened by the stress response via the elevated corticosteroid hormones (the stress hormone ACTH stimulates cortisol release from the adrenal glands). The stress of social isolation is also contributing to the weakening of the immune system in older people.
4. Exercise moderately and your immune system will get strengthened. Over exercising should be avoided as too much cortisol is released from your adrenal glands, which is toxic to lymphocytes thus weakening your immune system.
5. Socializing is good for you as studies have shown that you live 2 ½ years longer. This study here is from Connecticut, but other studies confirmed this as well.
6. Make love. The endorphins that are released in the process stimulate the immune system.
7. Take probiotics, because they help your gut flora to stay normal. A normal gut flora promotes a stronger immune system as the Peyer’s patches (clumps of immune cells) in the gut wall are intimately linked to the immune system. In this way probiotics indirectly support your immune system.
8. Avoid smoking. Smokers have more upper and lower respiratory tract infections than non-smokers. Here is information that explains this as well.
9. Get enough sleep. The circadian rhythm of your hormones ensures that your hormones function at their optimal level. Melatonin from the pineal gland is important in triggering the circadian rhythm, but melatonin itself supports the immune system as well. Your adrenal glands need resetting overnight so that cortisol is secreted according to your stress level, not too much and not too little. Overstimulation from performance sports, grief reactions, car accidents, injuries etc. lead to a surplus of cortisol and weakening of the immune system.
10. Take your flu shot (but without thimerosal) every year, but take it as a single shot (without thimerosal as a preservative). This CDC link explains that single shot flu vaccines are available without thimerosal. I recommend this type of flu vaccine. The central nervous system is extremely sensitive to nanograms of mercury, and it is for this reason that I would not buy into the argument of the CDC that one should not be concerned about safety of thimerosal. The newest for this flu season is the quadrivalent (or four-strain) flu vaccine, which is now available in pharmacies throughout the US.
11. Vitamins and supplements support your immune system, particularly vitamin D3. DHEA, which is available over the counter in the US stimulates antibody production when the flu vaccine is given, particularly in the elderly, in other words DHEA strengthens the immune system Vitamin C is known to support the immune system and is rapidly depleted in those who suffer from any viral infection. There are other nutrients that are useful to stimulate your immune system.
12. Consider herbs: Echinacea, Siberian ginseng, Asian and American ginseng, astragalus, garlic, and shiitake, reishi (also called “lingzhi mushroom”) and maitake mushrooms have all been shown to stimulate the immune system with negligible side effects.
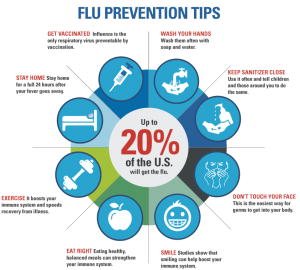
13. Wash your hands, particularly when there is a flu going around. Door knobs for instance are known to keep live viruses for 2 to 8 hours, so washing your hands will reduce the amount of virus you are exposed to.
Conclusion
There is no single solution to prevent the flu, but we can all minimize our exposure to the virus and strengthen our immune system. Although it is wise to get a yearly flu shot to boost your immune system (without thimerosal as a preservative) just before the epidemics come around, this alone is not as good as combining the non-specific factors mentioned here with it. Particularly vitamin D3 (2000 IU to 4000 IU per day) and the old stand-by vitamin C (1000 mg to 2000 mg daily) will stimulate your immune system. Spice up your dinners with mushrooms that stimulate your immune system (maitake, shiitake, reishi mushrooms). Go to bed early enough to allow your circadian hormone rhythms to be reset overnight as you sleep. This will stimulate your immune system (from melatonin and DHEA of your adrenal glands).
More info on the Flu: http://nethealthbook.com/infectious-disease/respiratory-infections/flu/
References:
1. Long: Principles and Practice of Pediatric Infectious Diseases, 4th ed. Prevention. Vaccine. © 2012 Saunders
Last edited Nov. 7, 2014