In February of 2001 my wife and I attended an anti-aging conference in San Diego. The keynote speaker was Dr. Barry Sears who is the inventor of the zone diet. We had read a book from him before the conference and were excited to hear him speak in person. We liked the book; we liked the talk, so we cut out sugar, starchy foods and stuck to a diet where the calories derived 50% from low-glycemic, complex carbohydrates, 25-30% from lean meat, poultry and fish. Calories derived from fat were reduced to about 15-20% (there is hidden fat even in lean meat). No butter, but instead some lean cheeses and olive oil for cooking and in salad dressings. We shed both 50 pounds within 3 months without any hunger pangs. Our energy increased and this has stayed this way ever since. There was no problem getting down with our BMI’s (body mass index) to 23.5 or 24.0, which is usually viewed as normal by the medical profession. We noticed, however, that when we did not exercise, there was a problem maintaining our normal weight. We are under the care of an anti-aging physician who did special tests like fasting insulin, C- reactive protein, and hormone tests. They were all normal. We took up ballroom dancing really seriously having been inspired by “Dancing With the Stars”. This was 6 years ago. What started innocently with only a few basic ballroom lessons three times per week has now blossomed into dancing more than 10 different dance styles 5 times per week.
3 ½ years ago both of our energy levels were slowly going down, particularly after a long night of dancing. Hormone tests revealed the initial stages of age-related hormone deficiencies which did not come as a surprise , as decreasing hormone levels was a topic discussed in detail at the conference in San Diego in 2001 (we also attended several other anti-aging conferences on a yearly basis from 2009 onwards). With bioidentical hormone replacements these levels normalized within one year, our energy was back and our weight stayed normal. We enjoy travelling, but there can be problems with our multistep weight management program. We need to watch our diet (no toxins, preferably only organic food), and physical exercise may be less regimented. In 2008 we read Suzanne Somers’ book “Breakthrough”. We ordered urine tests for toxic metals and we were shocked that we had noticeable levels of mercury and lead. Since then we started to cut our salmon consumption from 3 to 4 times per week down to once or twice per week. To get rid of the heavy metals we started intravenous chelation treatments with vitamin C (10 Gm) and Glutathione (1250 mg) every two weeks. In July 2012 there were reports of radioactive salmon from the Japan nuclear disaster earlier that year in the Canadian media. After this news we stopped eating all fish and other seafood, not only because of radioactivity, but also because of other toxins like mercury, cadmium, PBC’s etc. We do take high doses of molecularly distilled omega-3 fatty acids along with our other supplements. We also started eating mostly organic foods as we do not want to ingest insecticides, herbicides and other toxins.
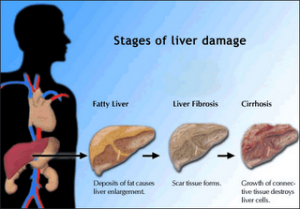
We acquired body composition scales, which give information about fat percentage including visceral fat percentage, muscle mass percentage, BMI, weight and the basic metabolic rate. We wanted to define the end point of what our ideal body weight would be. We noticed that our dance program was not good enough to lower the BMI below about 23.5; using the body composition scales we noted that our body fat content was still too high and the visceral fat percentage was still in the 6% range. It took a prolonged trip to the US where we could not find enough dance events to decide that we would introduce a one hour gym program consisting of 30 minutes of treadmill, 15 minutes of upper body circuits, and 15 minutes of lower body circuits every day as a basis to our exercise program. Any dance activity would be just an additional exercise on top of the base exercise from the gym. It took only about 2 months before our fat composition decreased, our muscle mass increased, the visceral fat went to a normal at 5% and the BMI was now stabilized at the 21.5 to 22.0 range. We feel a lot more confident in managing our weight long-term without really thinking much about the weight. It is now a routine we follow, like an athlete would do to stay in shape. While nobody has a permanent guarantee to everlasting health, we do it to prevent the diseases we do not need in our retirement like diabetes, arthritis, heart attacks, strokes, cancer or Alzheimer’s.
What we did not know until after the 20th A4M Anti-Aging Conference in Las Vegas (mid December 2012) was that inadvertently we were protected from exposure to chemically modified wheat from 2001 onwards as we had cut out all refined carbohydrates and starchy foods (including wheat) since then. Unfortunately many Americans still expose themselves unknowingly to larger or smaller quantities of wheat, suffer from leaky gut syndrome with the associated changes in the immune system and the development of autoimmune diseases.
Personally, I believe that long term weight management is possible: you can turn older and hopefully wiser…not wider. The good news: it can be done. The bad news: this is not an instant fix, but a program that needs to be part of your lifestyle package.
More information on weight loss: http://nethealthbook.com/health-nutrition-and-fitness/weight-loss-and-diet/
Last updated Nov. 6, 2014