Melatonin has been available to the public in the US since 1992. It is usually used as a sleeping aid or for jet lag related sleeping problems. However, in the last decade much more data about melatonin has come out that has proven that melatonin is a major hormone. The pineal gland contains another brain hormone, serotonin, which is converted into melatonin within that gland. Melatonin is a key hormone that regulates the sleep/wake cycle. It works in concert with cortisol, which has the highest level in the morning while melatonin has its highest level in the evening and during the night. Melatonin also regulates the menstrual cycle and determines when women get into menopause.
Lately new information has come to the forefront showing that there are connections to Alzheimer’s disease, Parkinson’s disease, stroke size and recovery from strokes. Even traumatic brain injury can be minimized when enough melatonin is present. In addition melatonin is an important anti-oxidant.
Finally, there is evidence that melatonin helps to determine how well we age.
In the following I like to review some of the evidence for all of these claims.
1. Melatonin as a hormone
Melatonin levels were found to be very low in breast cancer and prostate cancer patients. It has been determined that the immune cells have melatonin hormone receptors and need melatonin for stimulation. Because of the immune stimulatory effect of melatonin, it is often given as a cancer adjuvant treatment to other cancer treating modalities. Ref. 1 describes that melatonin regulates the female hormones (LH, FSH), which then determine when a woman has her menstrual period and also when she eventually enters menopause. The pineal gland is the master gland for the diurnal hormone rhythms.
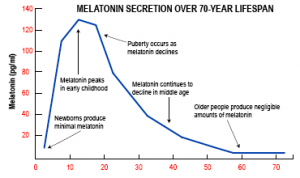
2. Melatonin levels decline with age
Melatonin levels in both men and women decline as we age. This figure shows that the highest melatonin levels are reached by the age of 10; by the age of 40 only 15% of the youthful levels remain while by the age of 55 only 5% or less of the original youthful levels are left. This explains why older people are more prone to infections (missing immune stimulation) and why the sleep pattern in older people is changed (shorter periods of sleep, less restful sleep). Ref. 1 points out that with insulin resistance (from diabetes or due to excessive sugar and starch consumption) cortisol levels are chronically elevated, which in turn inhibits melatonin production.
3. Melatonin protects from neurodegenerative diseases
A newer application of melatonin is as a preventative in the neurological field, particularly in the area of Alzheimer’s disease, Parkinson’s disease and the prevention of strokes. With respect to Alzheimer’s disease studies have shown that patients with Alzheimer’s have much lower melatonin blood levels when compared to age matched normal controls. In ischemic stroke patients it was found that stroke patients had much lower melatonin levels when compared to normal age-matched controls. Other studies have shown that pineal gland calcification was associated with low melatonin levels and a high risk for ischemic stroke. This risk was even higher when the patients had high blood pressure, diabetes and high cholesterol/triglycerides. When a stroke has occurred, it is important that the free radicals are removed as quickly as possible, which is where the antioxidant properties of melatonin fit into a rehabilitative program. The presence of melatonin enhances brain plasticity. However instead of using melatonin after a stroke, it is much better to use melatonin regularly before a possible stroke, as this gives a better chance reducing the size of the stroke. This in turn will lead to a faster and more complete recovery after a stroke.
Another important disease of the elderly is Parkinson’s disease. Melatonin helps to prevent oxidative damage to the dopamine producing cells in the basal ganglia thus preventing Parkinson’s disease. As with Alzheimer’s disease, there is a correlation of low melatonin levels and this neurodegenerative disease, which goes beyond the age-related reduction of melatonin levels. In experimental Parkinson’s disease models in mice melatonin was highly effective in preventing deterioration of Parkinson’s disease.
4. Melatonin may extend life
The combination of being a free radical scavenger, an immunostimulant and an integral key hormone allow melatonin to have beneficial effects in the aging process. When melatonin supplements are given, the stimulation of the immune system can cut down infection rates in the elderly, prevent and mitigate degenerative diseases of the brain (Alzheimer’s, Parkinson’s), re-establish sleep/waking rhythms and help reduce arthritis.
Conclusion
Melatonin is a widely used sleep aid. As it is practically absent in people beyond the age of 55, it makes sense to supplement with melatonin in that patient group. However, there are side effects particularly in people on blood thinners as coumadin competes with melatonin in getting eliminated through the cytochrome P450 liver enzyme system. This will result in longer bleeding times in patients on blood thinners who also take melatonin supplements. It is important that patients discuss this with their doctors. However, given all of the benefits described above, for the vast majority of the baby boomers melatonin supplementation would be very beneficial. Doses as a sleep aid vary between 1mg and 5mg at bedtime for most people. Cancer patients require higher doses (10 to 20 mg per day).
More information on melatonin, which is at the center of the circadian hormone rhythm as the key hormone switching from day to night and welcoming the day by switching its secretion from the pineal gland off in the morning: https://www.askdrray.com/how-to-cope-with-time-switches/
Reference
1. Datis Kharrazian: “Why isn’t my brain working?” Copyright 2013, Elephant Press, Carlsbad, CA, USA (pages 306-310).
Last edited Nov. 7, 2014