In the New Year it pays to backup your New Year’s resolutions by looking at short-term consequences. An article in “the conversation” explains how you can keep yourself motivated to stick to healthy habits. The alternative would be to fall back into unhealthy habits, which lead to various disease conditions. Traditional thinking centered around keeping long-term outlooks in front of your mind when tempted by the smell of doughnuts. In these cases, you think that the long-term consequences of eating doughnuts or consuming sugary drinks result in diabetes and obesity. But the smell or taste of unhealthy foods can be so overpowering that the long-term consequences of potential diseases is forgotten. This is the point when your New Years resolution may fade away in favor of falling back to unhealthy eating habits.
Think short-term to resist temptation
The new approach is to replace the thinking of long-term outlooks by short-term outlooks. The authors cited an example of 4000 participants in 7 separate studies. When the short-term consequences of anxiety and a sugar and caffeine crash were explained for caffeine containing sugary drinks, 25% of participants were able to abstain from the energy drinks in comparison to those who were informed about long-term consequences.
Another experiment
A similar experiment involved the consumption of sugar in the form of cookies. One group of participants read about the short-term effects of eating sugar. A second group read about the long-term effects of eating sugar. A third group did not get any information about the effect of sugar. There was also a “reward system” for all the participants: they had to decide between receiving a tote bag or eating cookies. Those who had read about the short-term effects of sugar were 30% less likely to choose cookies than the ones who read about the long-term effects. The ones who read the short-term effects were 45% less likely to choose the cookies than the ones who read nothing about the effects of sugar.
Verbalizing short-term consequences
Here are some thoughts that help to verbalize short-term consequences:
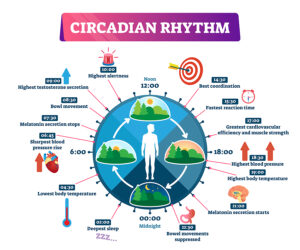
- For alcohol: excessive drinking can lead to poor sleep and hangovers.
- Fast food can make you feel bloated or give you indigestion.
- Sugar and starchy meals: make you bloated and give you an acidy stomach, also will lead to rapid weight gain.
- Focus on the good taste of apples and carrots. People will eat more of it and get the health benefits without mentioning it.
You can keep your goals easier when you combine them with small rewards here and there. When you have achieved one thing, you could watch your favorite TV show. Another reward could be a brief visit to the gym that makes you feel more fit. Or go and buy yourself a new pair of shorts for the gym. The authors of this article provide evidence from studies that showed that several mini rewards distributed throughout the day are more effective than big rewards at the end of the day.
Measurements of weight fluctuations
I found that body composition scales are very useful to monitor your diet intake. Here is an example how I use this device. My weights, fat% and body mass index for a number of days is listed below. The first line shows the baseline measured in the morning. On Saturday lunchtime I was invited to a Christmas family dinner. I ate more than I should have had. You can see the results on the Sunday readings: weight up, fat up and BMI up. I watched my calorie intake throughout Sunday.
Weekday Weight (KG) Fat % Body mass index
Saturday: 63.6 13.2 21.7
Sunday: 64.0 14.2 21.9
Monday: 63.4 14.3 21.7
It took another two days (Wednesday) before the fat percentage was down to 12.9.
There is another powerful tool, Dr. Valter Longo’s fasting mimicking diet. I reported about this under this link. Briefly, once a month I eat only 500 to 600 calories daily for 5 days. This helps me to lose my body mass index from 21.8 down to 21.1 or 21.2. After that I can eat a normal diet until the next month when I do the fasting mimicking diet again. It is an easy way to keep my body mass index in the 21.0 to 22.0 range. My wife and I prepare our own 500 to 600 calorie diet with natural food.(No, you do not get much, but it can taste good!) We do not buy Dr. Longo’s expensive diet boxes.
Conclusion
Focusing on short-term goals and consequences increases the percentage of success for those who have New Year’s resolutions. You can use this for many different approaches: eating less sugar, losing weight, getting regular exercise, reducing your alcohol intake, cutting out fast food and increasing your healthy vegetable and fruit intake. I also added a description of what I do with the help of body composition scales to control my weight and body mass index. I also use Dr. Longo’s fasting mimicking diet once per month for 5-days. Since December 2017 (for 6 years) I practiced this. I find it extremely useful to maintain my body mass index in the 21.0 to 22.0 range. Medicine knows that it is important to keep your body mass index below 25.0. This will prevent heart disease, type 2 diabetes and cancer. It also helps to look forward to a healthy New Year.