Dr. Filomena Trindade presented a talk about hormones helping in menopause. This talk was part the 26th Anti-Aging Conference of the American Academy of Anti-Aging Medicine in Las Vegas from December 13 to 15, 2018. The exact title of her talk was “Women and cognition: insulin, menopause and Alzheimer’s”. Above the age of 80 Alzheimer’s disease in women becomes much more common compared to men. PET scans of the brain of postmenopausal women in comparison to PET scans of premenopausal women, often show more than 30% slow down of metabolism after menopause. Literature regarding that finding showed that it was mostly the decline in ovarian estrogen production that was responsible for the slow down in brain metabolism. Other factors that lead to Alzheimer’s disease are central adiposity (abdominal) and inflammation in the body.
Brain insulin resistance and Alzheimer’s
Older women with Alzheimer’s have more IGF-1 resistance and IGF-1 dysfunction. Other studies showed that minimal cognitive impairment (MCI) progressing into Alzheimer’s disease (AD) might be due to type-2 diabetes. One of the studies stated the following:
“We conclude that the term type 3 diabetes accurately reflects the fact that AD represents a form of diabetes that selectively involves the brain and has molecular and biochemical features that overlap with both type 1 DM and type 2 DM.“
Another publication said that type 3 DM is a neuroendocrine disorder that represents the progression of type 2 DM to Alzheimer’s disease.
Dr. Trindade presented several hormone studies in postmenopausal women who started to develop Alzheimer’s disease. Older women with existing Alzheimer’s did not respond to estrogen hormone replacement. They did not recover with regard to their memory loss. However, younger women who just entered menopause responded well to estrogen hormone replacement and many recovered from their memory loss.
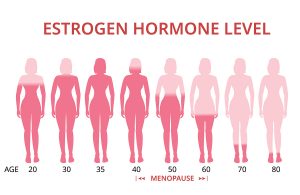
Hormone changes in menopause
There are a number of hormones that experience changes with the onset of menopause. Estrogen production ceases in the ovaries. The production of progesterone in the ovaries also ends. In addition thyroid and adrenal gland hormone production decreases. Often insulin production is increased, but insulin resistance is present at the same time.
Stress can interfere with progesterone and aldosterone production as pregnenolone is the same precursor molecule for both hormones.
How stress interferes with Selye’s general adaptation syndrome
Stage 1 of Selye’s adaptation syndrome, called arousal, involves elevation of cortisol and DHEA. When stress is over, the patient recovers on his/her own.
Stage 2 is the adaptation stage, where cortisol is chronically elevated, but DHEA is declining. The patient feels stressed, has anxiety attacks and may experience mood swings and depressions.
Stage 3 is the exhaustion stage. The underlying cause of this stage is adrenal insufficiency. Both cortisol and DHEA blood levels are low. Patients often suffer from depression and chronic fatigue.
Other hormones and menopause
DHEA and cortisol (stress) have the same precursor (pregnenolone). This means that when a patient is stressed, DHEA production tends to suffer as most of the pregnenolone is used for the production of cortisol.
Dr. Trindade spent some time explaining the complicated details of thyroid hormones during menopause. In essence stress can interfere with the normal metabolism of thyroid hormones with respect to T3, T4 and reverse T3. The end result is that not enough functioning thyroid hormones are present and hypothyroidism may develop.
Both estrogen and progesterone are lower in menopause. In a longitudinal French study with over 80,000 postmenopausal patients the women that received replacement with bioidentical progesterone and estrogen did the best in terms of low Alzheimer’s rates and lower heart attack rates. You achieve optimal Alzheimer’s prevention best starting hormone replacement at the time when menopause starts. You need both estrogen to control hot flashes and to give you strong bones, and progesterone for preservation of your brain, your hair growth and a good complexion.
Conclusion
Hormones are missing in menopause and this becomes the starting point for many postmenopausal complaints of patients. The sooner the physician does blood tests to diagnose hormone deficiencies, the better. Various studies showed that the best result in terms of Alzheimer’s prevention is possible, when estrogen and bioidentical progesterone are replaced right at the beginning of menopause. This approach prevents neuroinflammation. There are no extracellular beta amyloid protein deposits and no intracellular tau protein deposits that typically are present with Alzheimer’s disease. In addition the cardiovascular system stays healthier for longer. It contributes to preventing heart attacks and strokes. A longitudinal French study with over 80,000 women who have received treatment with a combination of estrogen and bioidentical progesterone have excellent survival data. The women also enjoy excellent mental health, no cardiovascular complications and less cancer than controls without hormone treatment.