The topic “about aging and a prolonged life” is always popular with people. CNN recently discussed this topic with the Nobel prize winner and molecular biologist, Professor Venki Ramakrishnan. He shared the 2009 Nobel Prize in Chemistry with Thomas A. Steitz and Ada Yonath for research on the structure and function of ribosomes. Ribosomes are sub particles in the cell responsible for making proteins. In the following I will summarize this interview.
What is aging?
150 years ago, people lived only about to 40 years. Today we can live up to 84 years in most countries. It is because medicine has learnt a lot about the reasons why diseases occur and how they can be cured. Physicians have a number of antibiotics available for those who suffer infections. Heart bypass surgeries and stents can prolong a person’s life when there is hardening of the coronary arteries.
Aging processes
The following aging processes occur all our lives:
- DNA breaks happen in our cells, but repair mechanisms are in place that deal with this. With older age repair mechanisms are more sluggish.
- Faulty proteins form inside cells, however, we have mechanisms to take care of that.
- Chemical damage to molecules in our cells accumulates. The cells can only partially eliminate these.
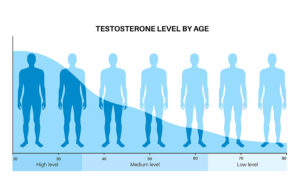
- Hormone disbalances occur during menopause and andropause. But anti-aging physicians can correct this by doing hormone tests and ordering bioidentical hormone supplements.
- There are limits of what anti-aging medicine can do: osteoarthritis affects our joints; our muscles are aging and with it our heart muscle. Degenerative neurological diseases like multiple sclerosis, Parkinson’s disease and dementia occur frequently as we get older with no effective therapies.
- The immune system weakens with age. To a certain extend vitamin D3 and other supplements can strengthen it, but only to a certain extent.
Systems working together in our body
Dr. Ramakrishnan said that our bodies work like cities. In it are various systems that need to work together to keep us alive. If a major system fails, we die. Some of the essential organ systems are the heart, the brain, kidneys, our gut, the lungs, the bone marrow and all our hormone glands. If one of these organs breaks down, we are in trouble. If an organ donor is not available, we perish. But even when everything is working together well, we are limited reaching a maximal lifespan of about 120 years. This has to do with limits of our cell metabolism and the aging processes mentioned above. Science has not found a way to prolong our maximal lifespan and likely will not find one soon. But there are various lifestyles that can prolong life as I mentioned here before.
Genetic effect on our lifespan
CNN asked Dr. Ramakrishnan what genetic effects there are that would transmit longevity from a parent who lived until 95 or older to a child’s lifespan. He answered the following: “There is a correlation between the ages of parents and their children, but it’s not perfect. A study of 2,700 Danish twins showed that heritability — how much of our longevity is due to our genes — only accounted for about 25% of lifespan. Still, researchers have found that mutation in just a single gene can double the lifespan of a certain type of worm. Clearly there’s a genetic component, but the effects and implications are complex.”
Relationship between cancer and aging
The same genes are involved for the growth of the body at a young age, and the older person who comes down with cancer. In old age the same genes can cause cancer and dementia. Dr. Ramakrishnan said: “Our risk of cancer increases with age because we accumulate defects in our DNA and genome, which sometimes cause gene malfunctions that lead to cancer. But many of our cellular repair systems that seem to be designed to avoid cancer early in life also cause aging later.”
Apoptosis (programmed cell death) and senescent cells
The body has two mechanisms in place that counter the danger of developing cancer cells. Dr. Ramakrishnan explained: “For example, cells can sense breaks in our DNA that might allow chromosomes to join in an abnormal way, which could lead to cancer. To prevent that joining, a cell will either kill itself or enter a state called senescence, where it can no longer divide. From the perspective of an organism like us, which has trillions of cells, this makes sense. Even if millions of cells are destroyed this way, these actions protect the whole organism. But the buildup of senescent cells is one of the ways we age.”
Lifestyle changes that help you live longer
Dr. Ramakrishnan said that our grandmothers knew what a healthy lifestyle was. The following is a list of what science now confirms adds years to your life:
- Don’t be gluttonous. Eating a variety of healthy foods in moderation can prevent the health risks of obesity.
- Get exercise: this helps us regenerate new mitochondria, which are the powerhouses of our cells providing energy.
- Avoid stress, which creates hormonal effects that change our metabolism and can accelerate aging.
More life prolonging points:
- Get enough sleep. This allows our bodies to do molecular-level repair.
- One of the newer findings is Dr. Longo’s fasting mimicking diet. Do a semi-fast once a month for 5 days with 500 to 600 calories per day. This helps you to shed 0.5 to 0.7 units of body mass index. It also stimulates your immune cells, your stem cells and elongates your telomeres. Long telomeres make you live longer.
- Replacing missing hormones with the help of an anti-aging physician will add about 10 years to your life. I mentioned this earlier.
A few more points about longevity research
Dr. Ramakrishnan said: “Already the top 10% of income earners in both the US and the UK live more than a decade longer than the bottom 10%. If you look at health span — the number of years of healthy life — that disparity is even greater. Poorer people are living shorter, less healthy lives.” He said further about the concept of “immortality”: “I think this quest for immortality is a mirage. One hundred and fifty years ago, you could expect to live until about 40. Today, life expectancy is about 80, which, as author Steven Johnson has said, is almost like adding a whole extra life. But we’re still obsessed about dying. I think if we lived to be 150, we’d be fretting about why we’re not living to 200 or 300. It’s never-ending.”
Conclusion
CNN discussed the quest for longevity with Nobel prize winning Dr. Ramakrishnan. He pointed out that the aging process is due to a number of factors that work together. There are DNA breaks, faulty proteins, chemical damage to molecules, hormone disbalances and degenerative changes. We need to watch that we do not overeat, get regular exercise and eat a variety of healthy foods. In addition, we need to avoid stress, get enough sleep and replace missing hormones with bioidentical hormones. A newer boost to your health is the fasting-mimicking diet (FMD) from Dr. Valter Longo that helps you keep your weight in the lower body mass index range. Dr. Longo showed in animal experiments and with humans that the FMD elongates telomeres, which directly prolongs life.
Apply what helps your longevity
While it is far-fetched to believe that we now have a ticket to live for 120 years or longer, it is more important to know that we can do our part to spend our golden years in health and wellness.