Lovastatin (Mevacor, from Merck) was the first statin drug approved by the FDA in 1987 as a cholesterol-lowering drug in the US. It made history in helping high-risk heart attack patients reduce their cholesterol levels and has helped safe many lives. But with the detection around 2002 that heart disease is an inflammatory disease, and that measuring the C-reactive protein with a blood test was a better than measuring cholesterol levels in predicting who would be at risk for developing a heart attack, the landscape has changed. Lifestyle changes have also been shown to be very effective in reducing cholesterol, C-reactive protein and triglyceride levels. In fact, lifestyle changes will reduce the risk for heart attacks and strokes. The newest flurry of activity with calls for putting more people on statins makes me suspicious that there could be a misrepresentation of the facts.
In this blog I am analyzing the literature to get to the bottom of the facts on reducing risk for heart attacks and strokes. I also come to my own conclusion.
Facts about cholesterol
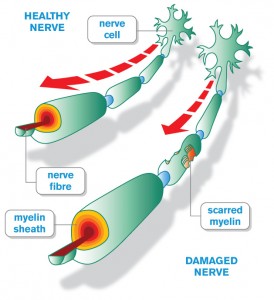
Cholesterol is a waxy substance that is part of the cell walls and plays a vital role in our metabolism. Liver cell membranes, for instance contain about 30% cholesterol. However, most of the cholesterol in our body comes from metabolism, 20 to 25% from the liver, the rest in the gut, adrenal glands and the reproductive organs, and also from the brain (the myelin sheaths contain a lot of cholesterol). 50% of the body’s cholesterol is recycled through bile salts and reabsorption of cholesterol in the gut (called the enterohepatic pathway).
Cholesterol is vital for cell function, for insulation of nerve fibers (myelin sheaths) and for synthesis of our steroid hormones (sex hormones and vitamin D3, which is now considered to be a hormone). The medical establishment took most of the information regarding heart attack and stroke prevention from the ongoing Framingham study. This clearly pointed to the importance of lowering the LDL cholesterol fraction (the “bad” cholesterol) and maintaining or increasing the HDL fraction (the “good” cholesterol). When it was realized that concentrating only on lowering cholesterol missed 50% of all heart attacks that researchers refocused and found the missing link, namely inflammation. Inflammation is at the cause of heart attacks and strokes, high cholesterol and lipids were only secondary phenomena. Ref. 2 points out that a comprehensive approach to treating a patient with high cholesterol should involve a combination of treatments aimed at the underlying risk factors for heart disease or stroke in a particular patient. This involves sophisticated blood tests where a metabolic derangement can be pinpointed. It should include measuring cholesterol fractions, lipids, the C-reactive protein, hormone levels and more.
How the traditional thinking about cholesterol has changed
The Framingham study has provided the basis for the drug industry to produce statins until about 2002 when our thinking about cholesterol being the culprit for causing heart attacks has forever changed. Subsequently further research showed that other factors like inflammation of the blood vessels, the metabolic syndrome associated with obesity and lack of exercise were also to blame for causing heart attacks and strokes. Recently more details have come to light, which point to multiple causes like the consumption of too much sugar, too much trans fats, too much salt and eating too much over processed convenience food. We end up gaining weight, develop the metabolic syndrome and inflammation of arteries (including the coronary arteries of the heart and the brain vessels). It is the lack of nitric oxide in the lining of the arteries, which combined with inflammatory substances from visceral fat are responsible for hardening of the arteries as the ultimate consequence of faulty nutrition and lack of exercise. We also know that oxidized LDL, particularly the very low-density lipoproteins (VLDL), will release free radicals and damage the arterial walls. CoQ-10 is a supplement, which is known to counteract this. One important test that had developed out of the Framingham study is the “ratio of total cholesterol to HDL cholesterol”, which is used by cardiologists to determine the risk of coronary artery disease. The average risk of this ratio for Americans is 5.0 for males and 4.4 for females. The ideal ratio to strive for is the “1/2 average risk” ratio of 3.4 for males and 3.3 for women (Ref.2). A fit, slim person who eats a low carb, normal fat diet (modified Mediterranean diet) will often have a ratio of only 3.0, well below the 1/2 average risk. The moment you introduce grains in your diet (cereals, bread, pasta) your liver will convert carbs into LDL cholesterol, while HDL cholesterol will drop resulting in a high risk ratio of above 5.0 (often 7 or 8 or more). The LDL will get oxidized and is deposited into your arteries setting you up for coming down with a heart attack or stroke down the road.
How do statins work?
The statins are a group of drugs that inhibit an enzyme, called the hydroxymethylglutaryl–Coenzyme A (HMG-CoA), which leads to a lowering of cholesterol, specifically a fraction known as the LDL cholesterol. The success story of lovastatin (Mevacor) led to a flurry of new HMG-CoA reductase inhibitors (cholesterol lowering drugs) such as fluvastatin (Lescol), pravastatin (Pravachol), simvastatin (Zocor), atorvastatin (Lipitor), and rosuvastatin (Crestor) in the late 1980’s and the 1990’s. Collectively it is now a 26 billion industry in annual sales.
Later investigations showed that there were other mechanisms by which statins helped, namely they were found to decrease the inflammatory reaction, which can be measured by lowering of the C-reactive protein. However, there are significant side effects in about 1 to 3% of people who take this medication, particularly an inflammation of liver cells (evident from elevation of liver enzymes) and a myopathy, which is a painful muscle condition (Ref. 1). This latter fact, which can occur in as many as 33% of the population at large (particularly the exercise minded) has limited the use of statins in competitive athletes where myopathies can occur in as many as 75% of athletes treated with statins (Ref.2). The reason for that is that the muscles of athletes cannot keep up with the demands put on them when they are kept in check by the HMG-CoA reductase inhibitors. On the other hand statins have prevented heart attacks and deaths from heart attacks and strokes in about 25% to 35% of patients treated with them as many clinical trials have shown (Ref.1), but simple supplements that have no side effects can do the same or do even better (see below).
The lack of cholesterol synthesis by the body’s cells when statins are given, leads to an expression of more LDL receptors on the cell surfaces. LDL binds to these receptors and enters the cells, which removes the circulating high risk LDL fraction of cholesterol from the blood thus causing a drop in LDL cholesterol. All of the side effects of statins (pull down to side effects in this link) can be explained as a result of the slow-down of organ functions (brain, muscles, gut, adrenal glands, etc.) as cholesterol synthesis is reduced.
New information from the Framingham Heart Study
So far everything I said made sense. But when I came across Ref. 4 I noticed that there was a bombshell of new information from another follow-up study of the Framingham Heart Study (Ref. 5) that did not fit in with the latest marketing drive of the statin manufacturers. In this study from 2005 Boston researchers had studied the outcomes of 789 men and 1105 women over a period of 16 to 18 years with respect to cognitive function. Participants were divided into total cholesterol groups that showed levels that were desirable (less than 200), borderline (200 to 239) or high (above 240). The astounding results were that higher cognitive functioning as documented in multiple cognitive tests in these three groups showed the best performance in the group with the highest cholesterol and the worst cognitive test outcomes in the lowest cholesterol group, quite opposite of what was expected.
Another important piece of research (April 2013) comes from Spain where doctors followed a group of 7447 patients with a high cardiovascular risk who were put on a Mediterranean diet with olive oil, a Mediterranean diet with nuts or a regular diet. The end point was death from heart attack or stroke. After 4.8 years the study had to be interrupted as the Mediterranean groups showed a significant survival advantage over the group on a regular diet.
Ref. 4 cited literature evidence that statins cause a 48% increased risk in postmenopausal women who take statins to develop diabetes. It also cites compelling evidence that diabetes patients are twice as likely to develop Alzheimer’s disease within 15 years and are 1.75 times more likely to develop any kind of dementia in the same time period.
Dr. Seneff from the Computer Science and Artificial Intelligence Laboratory at MIT explains in great detail that statins effectively reduce cholesterol synthesis in the liver, which in turn starves the brain of one of its main nutrients explaining why patient develop Alzheimer’s disease and dementia as a result of statin treatment.
So, the lessons to be learnt from these clinical trials are that you want to offer your brain enough cholesterol and healthy fat to have a normal metabolism. Fortunately, what’s good for your heart is also good for your brain. Conversely avoid statins, if you can and try alternatives first. Ref. 4 explains that for years the experts had the wrong theory that low fat/high carb was what would be good for your heart and brain, but the opposite is true: what is good for your heart and brain is a high healthy fats/low refined carb diet.
Make sure that with your blood tests that fasting insulin is low (no insulin resistance), that the ratio of total cholesterol to HDL cholesterol is less than 3.4 (low risk for heart attacks or strokes) and that the hemoglobin A1C level is low (4.8 to 5.6%, ideally less than 4.5%), which means you are not diabetic.
How alternative treatment can save you from heart attacks
Lifestyle treatment through dietary intervention, moderate exercise, and weight loss has been somewhat neglected by mainstream medicine, but is now recognized in regular textbooks of medicine as first-line treatment (Ref. 3). Most patients can lower LDL cholesterol by 10 to 15% through a change in diet. High-risk patients with established heart disease (narrowing of coronary arteries) require a drop of 30 to 60% of LDL cholesterol; this high-risk patient group may need an addition of a statin. In patients with metabolic syndrome or diabetes high triglycerides are often present and will respond to decreased intake of simple sugars, alcohol, and calories (Ref.3). Total calorie intake should be adjusted according to what the weight is when weighed every day with the goal of reducing the weight when overweight or obese, but maintaining the weight when it is in the normal body mass index range (BMI of 20 to 25). The total fat intake should be around 25%-35% of the total calorie intake. Specifically, saturated fat needs to be less than 7% of total calories, polyunsaturated fat up to 10% of total calories and monounsaturated fat up to 20% of total calories. Healthy fats according to Ref. 4 are extra-virgin olive oil, organic butter, almond milk, avocados, olives, nuts, nut butters and cheese ( except for blue cheeses). Other healthy fats are sesame oil, coconut oil, and the oils found in seeds like flaxseed, sunflower seeds, pumpkin seeds and chia seeds. Note that trans-fats (such as in margarine and baked goods) are a “no-no” as it causes free radicals in your body, which would accelerate the hardening of your arteries. Complex carbohydrates from vegetables and fruit are the main source of total calories providing 50%-60% of the total calories. Fiber intake needs to be 20-30 grams per day. Protein intake should be about 15% of total calories. Fat should provide 25% to 35% of the total calories per day. Cholesterol intake should be less than 200 mg per day. You may want to consider the use of plant sterols (2 grams per day) to enhance LDL cholesterol lowering. Physical activity from moderate exercise should expend at least 200 kcal per day (better 300 kcal).
Which supplements prevent heart attacks and strokes?
There are several nutrients that have been shown to be powerful preventers of heart attacks and strokes. I will review them briefly here (based on Ref. 2):
1. Coenzyme Q10 (CoQ10): The cells lining the arteries are only working well when their mitochondria are working properly producing chemical energy in form of ATP. CoQ10 is an important component of the mitochondrial metabolism; it is also the only fat soluble antioxidant that gets absorbed into the LDL particles where it protects these from oxidation. Statins suppress CoQ10 synthesis, so patients on statins need to take CoQ10 supplements daily to counteract this. However, anybody who is healthy now should take CoQ10 as a daily supplement for prevention. I take 400 mg per day.
2. Vitamin E (tocopherols): this fat soluble vitamin is an antioxidant and has been praised in the past as being heart supportive, was subsequently bad-mouthed by some conservative physicians, but lately has been resurrected. It turns out that there are 8 different types of tocopherols, with the alpha tocopherol being the most known, but gamma tocopherol is the one you want to make sure you are also getting with your balanced vitamin E supplement every day as this is the one that is a powerful anti-inflammatory. Simply ask staff at your health food store for a vitamin E supplement with gamma tocopherol in it. Take 400 IU per day (of the mix).
3. Curcumin: This is a powerful heart and brain protector combining three different mechanisms in one; it is reducing oxidative stress, is an anti-inflammatory and counters the process that threatens to destroy the lining of the arteries. One study on healthy volunteers showed a reduction of 33% in lipid oxidation, a 12% reduction of total cholesterol and an increase of 29% of the protective HDL cholesterol when 500 mg of curcumin was taken only for 7 days (Ref.2). This is the daily dose I would recommend for prevention of heart attacks and strokes.
4. Polyphenols: Flavonoids are the largest group among the polyphenols contained in such common foods as vegetables, fruits, tea, coffee, chocolate and wine. Over 130 studies have been done on humans showing improvement of the lining of the arteries (endothelial functioning) and lowering of blood pressure. Polyphenol consumption has been associated with a lower risk of mortality from heart attacks. Eat a Mediterranean type diet or a DASH diet and you will automatically get enough polyphenols with your food. However, resveratrol, the powerful red wine polyphenol warrants a separate daily supplementation as it prevents LDL oxidation in humans (Ref.2). Take about 250 mg of it daily.
5. Niacin/nicotinic acid: This supplement comes as “flush-free niacin” and also as extended release niacin; it can raise the beneficial HDL cholesterol by 30 to 35% when higher doses of 2.25 grams per day are used. In a metaanalysis of 7 studies it has been shown to significantly reduce heart attacks and transient ischemic attacks (precursor syndrome before developing a stroke). Niacin can change the small particle LDL into a large particle size LDL, which is less dangerous. Niacin has also been shown to reduce oxidation of LDL, which stops the atherosclerotic process. For a healthy person 500 mg per day of flush-free niacin is adequate.
6. Fish oil (omega-3-fatty acids): Because heart attacks are due to an inflammatory process and high LDL cholesterol is thought to be only a secondary phenomenon, it is very important to have this additional tool of an important anti-inflammatory supplement. In the past it was still safe to eat fish fairly frequently per week. But with mercury, radioactive iodine from Japan’s leaking reactor and carcinogenic PBC’s all congregating in the ocean waters, it is no longer safe to consume fish in large quantities. The remedy to this situation is molecularly distilled (or pharmaceutically pure) EPA/DHA supplements. EPA stands for eicosapentaenoic acid or omega-3 fatty acid. DHA is the acronym for docosahexaenoic acid. Fish oil supplements at a dosage of 3.35 grams per day of EPA plus DHA were shown to reduce triglycerides by up to 40%, equally to Lipitor or even more effective, but without the statin side effects. The amount of the dangerous small dense LDL is also being reduced with fish oil. Fish oil supplements have reduced the mortality from heart attacks and strokes and led to a higher survival from non-fatal heart attacks. At the same time these preventative fish oil doses will also treat and prevent arthritis.
7. Other useful supplements: Soluble fiber from psyllium, pectin, beta-glucans and others have been shown in clinical trials to reduce LDL cholesterol by binding bile salts in the gut (interrupting the enterohepatic pathway). Plant sterols (usually sold as sterol esters) are recognized by the FDA as reducing the risk of coronary heart disease, if taken in high enough amounts (2.4 grams of sterol esters per day). There are other useful supplements like artichoke extract, pomegranate, soy protein, Indian gooseberry (amla), garlic and pantethine (vitamin B5) that have been proven to be of benefit in terms of prevention of heart attacks and strokes. It would be too lengthy to get into more details here.
Conclusion
Recently there was a review in a medical journal that demonstrated that clinical guidelines (in this case for clinical guidelines for lowering cholesterol) erred 40% of the times when measured against scientific tests as this link explains. When it comes to saving lives by preventing heart attacks and strokes, what is needed is a multifactorial approach that treats the multifactorial causes of cardiovascular disease. Just pushing for treating more people with statins as Big Pharma is attempting to do is not addressing the fact that cholesterol is needed for our metabolism and the synthesis of our hormones. It is much superior to use a combination of different approaches that overlap and thus potentiate each other in their effects excluding statins first. Exercise creates more nitric oxide production by the lining of the arteries, which opens up arteries and prevents spasms. A proper diet with as many of the proven vitamins and other support factors will control inflammation and oxidation of LDL cholesterol particles as explained. This will prevent heart attacks and strokes as has been shown in many clinical trials. Only patients who come from families with genetically high cholesterol or high triglycerides and those patients who had heart attacks and strokes should be exposed to statins as they are at a higher risk of developing a heart attack or stroke. They need all of the help they can get in addition to the lifestyle factors mentioned. Most other patients and the public at large will do quite well without statins (no side effects of diabetes, Alzheimer’s and muscle pains). And, yes, a diet high in healthy fats, but low in refined carbs is what your brain and heart need (the opposite of what you have thought, see Ref. 4).
More information about side-effects of statins (acute pancreatitis): https://www.askdrray.com/pancreatitis-can-occur-with-statin-use/
Lower cholesterol with Mediterranean diet: http://nethealthbook.com/news/mediterranean-diet-benefits-us-workers/
References
1. Bonow: Braunwald’s Heart Disease – A Textbook of Cardiovascular Medicine, 9th ed. © 2011 Saunders.
2. Life Extension: Disease Prevention and Treatment, Fifth edition. 130 Evidence-Based Protocols to Combat the Diseases of Aging. © 2013
3. Melmed: Williams Textbook of Endocrinology, 12th ed. © 2011 Saunders.
4. David Perlmutter, MD: “Grain Brain. The Surprising Truth About Wheat, Carbs, And Sugar-Your Brain’s Silent Killers.” Little, Brown and Company, New York, 2013.
5. http://www.psychosomaticmedicine.org/content/67/1/24.full.pdf
Last edited Nov. 7, 2014