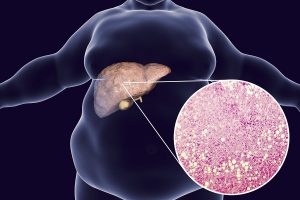
Non-alcoholic fatty liver disease (NAFLD) has been increasing in the general population. About 25% of all Americans suffer from this condition. It is more common among obese, overweight and diabetic patients. But it is also very common in people whose gut bacteria are abnormal. Antibiotic residues in red meat and in poultry can cause these gut bacteria changes according to scientists. Metabolic products of these abnormal gut bacteria are absorbed in the gut and end up in the portal vein. This is a large vein collecting all the nutrients and leaked toxins and transports them to the liver. The liver detoxifies toxins and digests nutrients. In the process the liver can get inflamed and turn into a fatty liver.
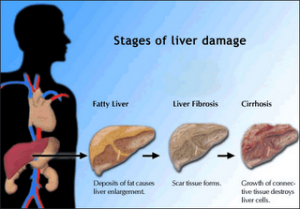
Fatty liver is still reversible
When liver damage continues, fibrotic changes can develop and liver cirrhosis is the next stage of this disease. Fatty liver is still reversible, but liver cirrhosis is not.
The January 2020 edition of LifeExtension magazine contains a review of non-alcoholic fatty liver disease (NAFLD). It also tells you what you can do to normalize the condition. In the following I am reviewing this article.
Probiotics can help to reverse non-alcoholic fatty liver disease
Two studies that I will describe in more detail later showed that probiotics can reduce inflammation in the blood significantly and can reverse fatty liver disease. Abnormal bacteria in the gut can also lead to leaky membranes of the gut wall. This can become permanent and the condition has the name “leaky gut syndrome”. Researchers have linked this condition to the development of autoimmune diseases. People with obesity and with high blood sugars (people with diabetes) have the highest risk of developing non-alcoholic fatty liver disease (NAFLD). The condition (NAFLD) does not produce any symptoms. But a combination of blood tests and scans can diagnose the condition.
Good and bad gut bacteria
If you allow the bad gut bacteria to stay, inflammation of the gut wall with leaky gut syndrome develops. This allows bacteria, toxins and other substances that should stay out of the blood to enter the body. Researchers have found that good bacteria can control the gut inflammation by taking probiotics, that will allow the leaky gut wall to heal. They found the following bacteria to be beneficial:
- Lactobacillus casei
- Lactobacillus rhamnosus
- Streptococcus thermophilus
- Bifidobacterium breve
- Lactobacillus acidophilus
- Bifidobacterium longum
- Lactobacillus bulgaricus
Probiotics usually contain most or all of these good bacteria. This allows the inflamed gut wall to heal and restore the gut barrier.
Two human trials
A randomized, double-blind, placebo-controlled clinical trial was published in 2014. 52 patients with NAFLD who were overweight or obese were taking probiotics twice a day versus a placebo control group. After 28 weeks the experimental group showed normalized liver enzymes and a significantly reduced C-reactive protein. The C-reactive protein was reduced by 54% in comparison to the placebo group.
The other clinical trial consisted of 50 patients with NAFLD, but a normal or low body mass index. Half of the patients were taking probiotics, the other half placebo pills. The researchers noted that after 28 weeks the inflammatory markers were much lower in the experimental group than in the placebo group. Also, the liver values were now normal.
Discussion
Patients with non-alcoholic fatty liver disease are in danger of progressing to liver cirrhosis and liver failure. At this point only a liver transplant could rescue them from death. However, as the clinical trials have shown, the use of probiotics to normalize the gut bacteria can normalize the inflammation of the gut and reverse fatty liver disease. Regular exercise and weight loss through the use of a lower calorie diet will also help in normalizing the liver function. When prebiotics are added to probiotics the healing effect is amplified even further. Prebiotics contain fiber that cannot be digested, but which is useful for bacteria from the probiotics to multiply on.
Conclusion
We need to pay more attention to the food we are consuming. For instance, regular beef in the US contains antibiotic residues that permanently change the gut flora. This leads to an inflammatory reaction of the gut wall and leaky gut syndrome. Gut bacteria and toxic substances can now enter into the portal vein and reach the liver. The liver attempts to detoxify this, but in the process, it also develops non-alcoholic fatty liver disease (NAFLD). About 25% of Americans have this condition, which is asymptomatic. The only way to diagnose it is through blood tests and scans. Two clinical trials have documented that NAFLD can reverse back to normal with the consumption of probiotics. Regular exercise and weight loss (calorie-reduced diet) also help to reverse NAFLD back to normal liver tissue. It is obvious that a timely intervention is necessary to avoid the progression to liver cirrhosis!