New cancer research suggests that chronic virus particles in beef and dairy may cause cancer and MS (multiple sclerosis). The Medical journal Medscape.com had a review article that summarized this line of research.
Papillomaviruses and cervical cancer
Harald zur Hausen, M.D., D.Sc., a German virologist, detected that papillomavirus causes cervical cancer. He was given the Nobel prize in Medicine in 2008 for “his discovery of human papillomaviruses causing cervical cancer”. In the meantime, we know that there are two strains, namely HPV-16 and HPV-18 that are carcinogenic. We also learnt that papillomavirus causes oropharyngeal cancer, anal cancer, penile cancer and vulvar cancer. Since then, HPV vaccines are commonly in use for cancer prevention.
Evidence for causation of colorectal cancer
Professor Harald zur Hausen and his wife, Professor Ethel-Michele de Villiers, continued work on looking for viral particles in many other cancers. This led them to state that colorectal cancer was due to a latent viral infection. He determined that, when women were breastfeeding their infants for prolonged periods of time (about 1 year), they transmitted oligosaccharides with the breast milk to their offspring, which gave lifelong prevention against colorectal cancer to their children. He also showed that colon cancer patients had round particles in their intestinal mucous membranes, which consisted of single-stranded DNA rings.
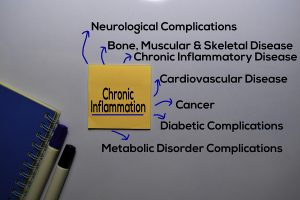
Persistent viruses
The researchers said that they came from viruses and they named them bovine meat and milk factors (BMMF). In the same areas in the intestine, they detected acid radicals from oxidative stress typical for chronic inflammation. They postulated that infants who are weaned from breast milk prematurely, and started on cow milk formulas ingest BMMF. This infects the lining of the gut where a chronic subclinical BMMF infection gets established. Decades later the patient comes down with colorectal cancer. They established that children who are breast fed for 1 year do not get BMMF particles in the lining of their guts or colorectal cancer. They also don’t get MS in adult life.
Criticism of two regulatory agencies in Germany
The above results of professor zur Hausen and his wife were published in February of 2019. This led to a lot of press releases questioning these results. In Germany the consumption of beef and milk products is popular. The DKFZ (Deutsches Krebsforschungszentrum) felt that an “all-clear signal” was necessary. The Bundesinstitut für Risikobewertung (BfR) stands for the German Federal Institute for Risk Assessment, situated in Berlin. It is a substructure of the German government responsible for food safety. The second agency is the Max Rubner Institute (MRI) in Karlsruhe, also known as Federal Research Institute of Nutrition and Food. Both agencies started to investigate the facts of Prof. zur Hausen’s research. At the end of November 2022 the BfR and MRI made a joint statement. They stated the following:
- BMMF were not new viral agents, but variations of already known DNA sequences.
- BMMF commonly occurred in a variety of animal- and plant-based foods.
- BMMF were not capable of infecting human cells.
- It was true that consumption of red and processed meat correlates with the incidence of intestinal tumors.
- However, consumption of dairy products are linked to a reduced risk of intestinal tumors.
- There is no evidence that breast cancer would be associated with the consumption of beef or dairy.
- They stated that milk products and beef are valuable supplementary diet components for infants due to their micronutrients. They further stated that dairy and beef products are safe for people of all ages.
Evidence for causation of multiple sclerosis
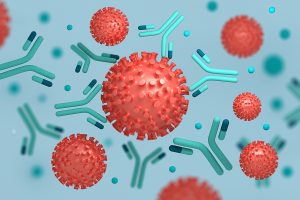
Professor zur Hausen and his wife, Professor Ethel-Michele de Villiers both worked at the German Cancer Research Center in Heidelberg. They pursued research about MS. MS is usually attributed to IgG1 and IgG3 autoantibodies that destroy Schwann cells. The Hausen research team found the following perplexing facts:
- MS was associated with the consumption of dairy products and beef products.
- They isolated ring-shaped DNA molecules (BMMF) from dairy and cattle blood.
- Epstein Barr virus (EBV) also plays a role in initiating MS. MS patients have higher antibody titers against EBV.
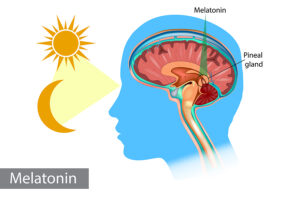
- One research paper noticed that MS patients in Antarctica secreted EBV in their saliva in the winter month. However, vitamin D3 stopped the viral excretion. This is very interesting as vitamin D is an important immune response stimulator.
More evidence:
- They isolated BMMF particles from lesions of MS patients.
- They noticed the old fact that MS is more common further away from the equator. Vitamin D production from sun exposure reduced cases of MS.
- Prolonged breast feeding up to one year prevents life threatening rotaviruses and noroviruses in the newborn. The reason is exposure to oligosaccharides in breast milk. The mother starts producing breast milk in the middle of her pregnancy. It protects mother from tumors (including breast cancer), from MS later in life as well as type 2 diabetes.
- The researchers formulated the hypothesis that both EBV and BMMF are responsible in patients to form MS lesions in the brain when vitamin D levels are low. A good dose of vitamin D3 every day may be helping to keep EBV and BMMF in a dormant phase.
Discussion
At this point there is no consensus why an increased consumption of beef and processed meat causes more colorectal cancer. The question is whether BMMF particles cause colorectal cancer or whether meat consumption experiences metabolization into carcinogenic substances? Either way it would be desirable to cut down on your red meat consumption.
With respect to MS, we know that autoantibodies are destroying the Schwann cells. But the question is why the immune system produces autoantibodies. Could it be that persistent EBV viruses switch the immune system from a normal to an autoantibody mode? Would BMMF be an additional factor?
Conclusion
Professor zur Hausen, a virologist from Germany and his wife Professor Ethel-Michele de Villiers researched persistent viruses. Professor zur Hausen detected the connection of papilloma viruses to cervical cancer. He received the Nobel prize in medicine 2008. They proposed the theory that newborns in their first year of life have an immature immune system. If they are fed cow’s milk and/or beef during the first year they accumulate bovine meat and milk factors (BMMF), which can subsequently lead to colon cancer or to MS as an adult. Two top German institutes banded together to criticize Prof. zur Hausen’s research.
Criticism of Professor zur Hausen’s research
The Bundesinstitut für Risikobewertung (BfR) stands for the German Federal Institute for Risk Assessment, situated in Berlin. It is a substructure of the German government responsible for food safety. The second agency is the Max Rubner Institute (MRI) in Karlsruhe, also known as Federal Research Institute of Nutrition and Food. These research institutes concluded that not all of the findings of Professor zur Hausen were valid. I listed 7 of their concerns. On the other hand, they agreed that it was true that consumption of red and processed meat correlated with the incidence of intestinal tumors. Time will tell which parts of the research ultimately will be valid and which are not.