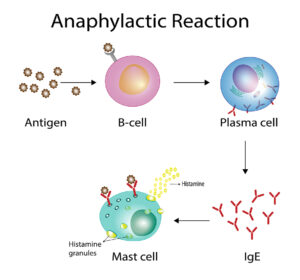
Mast cell activation syndrome (MCAS) also goes by the name of systemic macrocytosis. That is to say it is a syndrome where mast cells are multiplying abundantly and secreting the inflammatory substances histamine, leukotrienes and cytokines. Certainly, people who suffer from MCAS can get severe anaphylactic reactions, but an epinephrine injection can often stop this. Indeed, the physician must look for potential triggering factors like alcohol, spicy foods, exercise, insect stings, possible heavy metal accumulation or certain medications. In some cases heavy metal accumulation could also be a factor that triggers mast cells to release histamine. In these cases a series of 20 chelation therapy sessions would be stabilizing.
Symptoms of mast cell activation syndrome
- When there is skin involvement in patients with mast cell activation syndrome, they get flushing, itching and skin rashes.
- With gastrointestinal involvement patients experience nausea and vomiting, bloating, abdominal pain, diarrhea and reflux (GERD).
- Patients with neurological symptoms develop brain fog, headaches, cognitive problems, tremors and anxiety/depression.
- When MCAS affects your endocrine glands, you may develop bone pain, bone lesions or weak bones.
- Patients where the heart is affected may be fainting, their blood pressure may fluctuate between with high or low readings and they may experience heart palpitations.
- When your respiratory system is affected, your lungs may be wheezing and you may develop nasal congestion.
- More symptoms
- The most dangerous symptom is anaphylaxis. This is a life-threatening allergic reaction where your air way entry could close off.
- Any of these symptoms can get triggered by heat, cold or temperature changes. Stress, friction, insect bites or stings can also trigger a reaction. Additional factors can be environmental odors or perfumes, certain foods or medicine, alcohol and contrast dyes.
Diagnosis of mast cell activation syndrome
The most appropriate specialist to see is an allergist or immunologist. Other specialists could be a dermatologist, gastroenterologist, hematologist or endocrinologist. You will need blood tests like a serum tryptase level, which is a marker for mast cell burden. It is best to get a baseline tryptase level and also get a tryptase level after a mast cell reaction. In addition, you need a 24-hour urine collection for a number of mast cell activators. Depending on where your mast cell activation syndrome is located you need a skin or bone marrow biopsy.
More possible tests
The physician may decide to do an endoscopy or colonoscopy of the gastrointestinal tract. The pathologist can do several staining procedures with biopsy material to specifically look at mast cells. If there is a strong family history of mast cell activation syndrome the physician may decide to do genetic tests. In order to assess mast cell damage, your doctor may order a bone density test and bone scans including CT scans of the abdomen and chest.
Treatment of mast cell activation syndrome
The treatment of mast cell activation syndrome consists of a combination of multiple steps. First, if there is a life-threatening anaphylactic reaction, the patient applies an epinephrine injection. The physician taught the patient earlier how to do an epinephrine injection. This stops the sudden, rapid release of mediators from mast cells. After the epinephrine injection the patient needs transport to the nearest ER of a hospital for follow-up care. It is important that any patient with this syndrome should carry injectable epinephrine( an Epi-Pen) at all times.The purpose of treatment against mast cell activation syndrome is to block reactivity of mast cells or to stop the effects of mast cell mediators.
A number of medications are available to do this.
- H1 and H2 antihistamines. The difference between these two is explained here.
- Mast cell stabilizers (cromolyn sodium, ketotifen). For more on ketotifen follow this link.
- Leukotriene inhibitors such as montelukast. You can find more info on leukotriene modifiers here.
- Aspirin (under direct physician’s supervision)
- Aggressive mast cell disease may require treatment with chemotherapy.
You can lower your risk of getting mast cell activation syndrome by watching your diet. Here is a list of the foods that will protect you:
Conclusion
Mast cell activation syndrome is a complex disease entity. Often there are several factors that contribute to this. Conventional medicine still cannot offer a treatment modality that will cure this condition, the only possibility is to control it. The physician must therefore use a combination of treatment modalities in order to help the patient with this condition. In cases of heavy metal accumulation several treatments with chelation therapy are beneficial. With an acute anaphylactic reaction, the
Mast Cell Activation Syndrome applies an epinephrine injection, which will stabilize the condition. But the patient should now follow this up with a series of blood tests in the emergency department of a hospital.
Treating mast cell hyperactivity
The purpose of treating mast cell activation syndrome is to block reactivity of mast cells or to stop the effects of mast cell mediators. H1 and H2 antihistamines help for gastrointestinal hyperactivity. Cromolyn sodium and ketotifen are mast cell stabilizers. Leukotriene inhibitors such as montelukast help to stabilize the mast cells to not secrete cytokines, which cause inflammation. Aggressive mast cell disease may require chemotherapy treatment, similar to what is needed to treat cancer.
The purpose of treatment is to help the patient control the mast cell hyperactivity. At this time medical science does not have all the answers. Unfortunately, at this point conventional medicine has no cure for this syndrome, but it can be managed with a lot of attention to the symptoms.