Toxic levels of formaldehyde in laminate wood flooring were underestimated, concealing the hazards of formaldehyde. Specifically, laminate wood flooring produced in China and sold by Lumber Liquidators, based in Toano, Virginia were identified as a problem.
News about the hazards of formaldehyde in Chinese laminate flooring
Last year CBS ran a story with Anderson Cooper regarding Chinese imported laminate flooring that emitted more than the stated amount of toxic formaldehyde. This was based on independent testing by CBS. Examiners found that laminate packages released between 6 and 7 times the amount of allowable formaldehyde. Moreover, some packages of the cheap Chinese made laminate flooring even released 20 times the allowable amount.
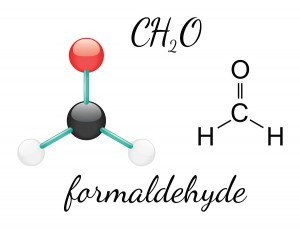
Certainly, formaldehyde is part of the glue in use to bind the wood particles together to make the laminate flooring. The laminate top seals the wooden core and keeps most of the formaldehyde inside.
Formaldehyde leaks into the home slowly
But over time it gradually leaks into the home. It is a matter of how much formaldehyde was in the glue and how good the ventilation of the home is, which determines the concentration of formaldehyde in the air.
CBS bought 31 boxes of the Chinese-made laminate flooring that Lumber Liquidators was selling in Virginia, Florida, Texas, Illinois and New York. The examiners sent samples to two reference labs. Most noteworthy, only one package was compliant with formaldehyde emissions standards. Some were more than 13 times over the California limit. Both labs were surprised how high the readings were, as they had not encountered this when they tested regular laminate flooring before.
Effects of the hazards of formaldehyde
Dr. Philip Landrigan at N.Y.’s Mt. Sinai Hospital specializes in environmental pediatrics and exposure to toxic chemicals. He stated that what matters is the concentration of formaldehyde in the typical home where such a floor is installed. Nevertheless, it needs to be stated that these toxic levels were only found in the cheap flooring of the above named company and this product has since been removed from the market. Above all, formaldehyde is a known carcinogen (cancer producing substance). As a matter of fact, it irritates the airways, particularly in individuals who are sensitive like asthmatics.
Toxic effects on immune system of formaldehyde exposed workers
A 2014 occupational medicine study from China compared factory workers exposed to formaldehyde with controls. Notably, they found higher formic acid levels in the urine of exposed workers. Formic acid is the end metabolic product of formaldehyde. In addition, they also had higher B cell lymphocyte counts (in the high dose exposure group) and higher natural killer lymphocyte counts (in the low dose exposure group). As a result, this would explain the toxic effects on the immune system and the higher incidence of cancer in formaldehyde exposed individuals.
DNA changes in mouth cavity cells and nasal cells of anatomy workers
A 2015 study from Portugal examined DNA abnormalities in cells from anatomy workers. Furthermore, anatomy workers who prepare corpses with formaldehyde for anatomy courses are under the exposure of formaldehyde fumes. Another exposure can happen when fixating histology slides with formaldehyde to get them ready for microscopic examination. The researchers measured the the formaldehyde concentration in the air of the anatomy lab as 0.38 parts per million. Likewise, genetic analysis of cells from the mouth cavity and nasal cells showed significant DNA abnormalities, while controls without formaldehyde exposure did not have such DNA changes.
Formaldehyde poisons p53 cancer suppressor gene
In this study there was insufficient data to link formaldehyde exposure to causation of leukemia. It is peculiar that on a molecular level it is clear what formaldehyde does to the p53 suppressor gene. But it is more difficult to show the link of formaldehyde exposure to the causation of a multitude of cancers.
WHO recommendation about formaldehyde
The WHO recommends keeping formaldehyde below 0.08 ppm in the air of factories where formaldehyde is used. WHO says that this will prevent nasal cancer and leukemia. Levels of 1 ppm can cause nasal cancer and leukemia in humans. The level for hardwood plywood is 0.05 ppm in the US since 2012
The CDC involvement in safe formaldehyde levels in the air of a home
The CDC faced with the problem of the Chinese laminate imports of Lumber Liquidators and did its own investigation. The conclusion was that these high concentrations of formaldehyde were not only affecting sensitive people, but in fact everybody. The CDC stated: “The lifetime cancer risk increased from the previous estimate of 2 to 9 extra cases for every 100,000 people to between 6 and 30 extra cases per 100,000 people. To put these numbers into perspective, the American Cancer Society estimates that up to 50,000 of every 100,000 people may develop cancer from all causes over their lifetimes.”
New guidelines for the limit of formaldehyde in residences
New guidelines for the limit of formaldehyde in residences were defined as 135 µg/m³ by the National Center for Environmental Health. This is a different nomenclature for formaldehyde concentration in the air and I will show the conversion to parts per million particles in a moment. This reference explains that 1 ppm = 1.23 mg/m³. 135 µg/m³ is the same as 0.135 mg/m³. When you divide 0.135 mg/m³ by 1.23 mg/m³, you have converted this into 0.11 ppm, the upper acceptable formaldehyde limit. Had the company followed proper procedure, it is clear from the recommendation above that the formaldehyde level of 0.05 ppm was in the safe zone. It was much smaller than 0.11 ppm. The cheap batch of plywood discussed above with the high formaldehyde glue gave measurements much higher than any of these guidelines.
Company response to bad publicity regarding “the hazards of formaldehyde”
As the stock of Lumber Liquidators plunged, the company decided to do something about this. In May of 2015 they stopped the sale of the cheap laminate products. It turned out that they had been poor quality, cheaper laminate boards; the producer had used glue with too much formaldehyde in it. The company had knowingly bought these for a 10% discount and hoped to make a huge profit through its over 360 stores in 46 states. Before this fiasco revenue was more than a billion dollars a year. Now the company tries to rescue its brand name through an ongoing painstaking public relations effort.
What to do, if you own cheap laminate flooring with the hazards of formaldehyde?
The CDC says you should ventilate the home, use additional vents to remove bad air, keep the temperature at the lowest comfortable setting and make your home a smoke-free home.
Many homeowners have ripped out the cheap laminate flooring and replaced it with better quality products and joined a class action suit against the company that sold them the product. Others leave it in place, open the windows and doors more frequently to keep the air concentration of formaldehyde lower; and they follow the other suggestions from the CDC.
According to this update formaldehyde levels are decreased significantly 6 to 10 months after initial installation.
Conclusion
Had Lumber Liquidators not been greedy for profit, we may never have known the story of formaldehyde overdosing of glue in one bad batch of laminate flooring. The unsuspecting consumer got a special deal, but nobody informed the consumer about the hazards of formaldehyde release! Keep in mind that not everything that is cheap is good quality.
Only a few years back urea formaldehyde was very popular as a means to insulate your home. Homeowners soon found out that this could lead to toxic formaldehyde fumes and they had to replace urea formaldehyde with glass fiber insulation.
Never sit back and think you are safe
You may not have to panic. Frequent ventilation, as described, can lower the formaldehyde concentration in the air. And eventually in the case of laminate flooring the concentration is low enough from the passage of time that there is no longer a danger from leaking formaldehyde gases.
What I have learnt from this is the following: never sit back and think you are safe. Watch what you are eating. Watch what you are drinking. Women, watch what cosmetics you put on your skin. Be aware of the potential hazards of fire retardant in textiles and noxious substances in building products. All of this can impact the quality of the air you are breathing!