Dr. Michael Nova gave a talk about the role of genetic switches to treat obesity and diabetes. He gave this talk as part of the 24th Annual World Congress on Anti-Aging Medicine (Dec. 9-11, 2016) in Las Vegas that I attended. The full title of the talk was “Nutritional Genetics and Epigenetics in Diabetes and Obesity Management”. Dr. Michael Nova is the Chief Innovation Officer at Pathway Genomics, San Diego, CA 92121.
Twin studies are a powerful tool to show that longevity is both genetically caused as well as environmentally.
In the light of these studies the results showed that 80% of a long life (longevity) is due to a healthy lifestyle and 20% comes from genetics. In addition, there are powerful epigenetic factors that can slow down aging and that can interfere with the inflammatory process that causes heart disease, obesity and diabetes. Also, there are specific inflammatory markers, which blood tests can determine. As a matter of fact, one of the first inflammatory markers detected was the C-reactive protein.
What diseases are caused from inflammation?
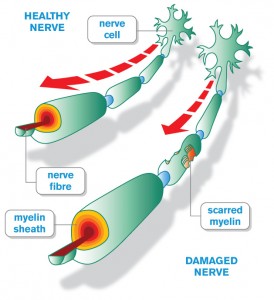
Dr. Nova showed a slide depicting MS and Alzheimer’s disease. In the heart area atherosclerosis was shown to cause heart attacks and strokes. Next diabetes, lupus, obesity and irritable bowel disease were depicted. Finally there is arthritis that interferes with joint movements. In other words, all of these conditions have inflammation at the core, which leads to worsening of the conditions, if the inflammation is not stopped through nutritional or medical means.
Age-related diseases also due to inflammation
Furthermore, inflammation is not only confined to these conditions. Research has shown that the following age-related diseases belong into the inflammatory category. These are: osteoporosis, depression, diabetes, cancer, neurodegenerative diseases (Parkinson’s disease, Alzheimer’s), asthma, central obesity, metabolic syndrome and cardiovascular disease. In these diseases the C-reactive protein is often up, so is the fasting insulin level. The rest of the talk concentrated on how various changes in food intake and supplements could lead to epigenetic changes that improve the patients’ conditions.
Human genetics are complicated
The speaker mentioned how complex the human genetics are, and he showed a number of slides that are too complicated to discuss here. There are unstable genes, which can become important in the development of illnesses, particularly when you don’t exercise and you eat a Standard North American diet. There are genes involved that cause diabetes, but they need environmental triggering to get expressed. Dr. Nova showed one slide that listed two genetic variants, which when activated by inflammation rendered the person positive for diabetes or heart disease. On the other hand, if inflammation is vigorously treated with a Mediterranean diet and Metformin, the hemoglobin A1C will decrease to less than 6.0% and diabetes will disappear.
Obesity and genetic factors
Obesity has a 40% to 60% hereditary rate. The fat mass and obesity-associated gene, FTO gene for short is the reason some people gain weight. When this gene is not present, the person has no problem maintaining a normal weight. The FTO gene is located on chromosome 16. Moreover, there are other genes with complicated names that can also increase weight.
It is important that there are many factors that work together in developing obesity. Dr. Nova called this the “epigenetic modulation”. He explained further that there are at least 12 factors working together that can reduce obesity. These are:
- Diet
- Diurnal/seasonal correlations
- Smoking and other toxic chemicals
- Street drug use
- Disease exposure
- Financial status
- Exercise status
- Microbiome healthy?
- Therapeutic drugs
- Alternative medicine
- Social interactions
- Psychological state
First, low carbohydrate diets and the ketogenic diet are helping to reduce weight. Second, financial stress leads to more cortisol production, which leads to weight gain. Third, an unhealthy bacteria composition in your gut causes you to gain weight, while a good composition of bacteria helps you lose weight. Furthermore, overcoming depression with cognitive therapy can help reduce your weight. Those are just a few examples in more detail from the list of 12 factors.
Extensive research has shown that genetic factors and environmental factors interact to lead to epigenetic marks or imprinting. It is important to realize that epigenetic factors have an influence on gene expression, but they don’t change the underlying DNA sequencing.
As can be seen, there are still gaps of knowledge how obesity develops, what percentage is due to genetic factors and how much is due to other factors including diets.
Diabetes and genetic factors
Nutrition can influence major metabolic processes in our body cells like phosphorylation, acetylation and methylation. This allows epigenetic mechanism of actions to interfere with the expression of inherited health problems like diabetes and other diseases. This has the potential to improve quality of life.
Useful supplements
Dr. Nora showed a slide with a number of useful supplements.
- EGCG is the effective component of green tea. It supports the viability of the beta-islets of the pancreas that produce insulin. It leads to more secretion of insulin.
- Naringin and Hesperidin decrease high blood sugar levels.
- Anthocyanin decreases high blood sugar levels.
- Quercetin increases cell proliferation in the liver and the pancreas.
- Vitamin D3 reduces diabetes incidence and inflammation of the insulin-producing cells.
- Biotin in combination with chromium increases insulin secretion and lowers blood sugars.
- Vitamin B2, also known as riboflavin has anti-inflammatory effects.
- Alpha-lipoic acid protects against diabetes by reducing blood sugar levels.
There are several genes responsible for the development of type 2 diabetes, one of them is the FTO gene that is also important in the development of obesity. But Dr. Nora projected a slide that showed 14 other genes that may lead to the development of diabetes. I have elected to not get into all of those details.
What Dr. Nora concluded is that healthy nutrition plays a vital role in preventing FTO gene expression. He talked about silencing genes, which good nutrition and supplements can do.
Silencing diabetes genes
A Mediterranean diet can stabilize the metabolism and fight inflammation. In like manner zinc and magnesium are important cofactors in enzymes necessary to prevent diabetes. In the same fashion Vitamin D3 and omega-3 intake are helping to control inflammation and preserve beta cells in the pancreas in diabetes patients.
Nutritional genetic modifiers
Foods that methylate DNA and silence genes are: citrus (hesperidin), apples (phloretin) and tomatoes (lycopene). The following foods do both DNA methylation and histone modifications: turmeric (curcumin), cinnamon (coumaric acid), green tea (EGCG), soybean (genistein), coffee (caffeic acid) and broccoli (isothiocyanates). These three foods only do histone modifications: garlic (allyl mercaptan), grapes, (resveratrol) and cashew nuts (anacardic acid).
Functional foods with regard to obesity and diabetes
Here are a few food items and their effects on your health.
- The lignans of flaxseed lower LDL cholesterol and total cholesterol.
- The catechins of green tea prevent obesity, but also obesity-induced type 2 diabetes.
- Saponins of fenugreek lower lipid peroxidation and increase the antioxidant level.
- Soy proteins contain phytoestrogen, genistein and daidzein; this lowers cholesterol levels in the blood, prevents lipid peroxidation and also has antioxidant activity.
- Banaba leaves extract contains corosolic acid and ellagitannins. These substances are able to lower glucose levels in the blood. It also has an anti-obesity effect.
- Grapes and related products contain anthocyanin, flavan-3-ols and flavonols. They have blood pressure lowering qualities, lower blood fat levels and prevent hardening of the arteries.
- Dark chocolate contains flavanols that are the main type of flavonoid found in it. Flavanols decrease blood pressure and make platelets in the blood less sticky. This prevents heart attacks and strokes. In addition these flavanols also decrease LDL cholesterol, which prevents hardening of the arteries.
Here are more items that help your health
- Red wine, berries, pears, and apples: proanthocyanidins are the active polyphenols that make all of these fruit valuable. Proanthocyanidins prevent LDL cholesterol from oxidizing through their antioxidant effects, which in turn slows down hardening of the arteries. It reduces the inflammation associated with narrowing of blood vessels and normalizes the lining of arteries.
- Onions contain two active ingredients, allyl propyl disulfide (which makes you cry when you cut onions) and S-methyl-cysteine sulfoxide. These substances have anti-diabetic effects and lower blood fatty substances.
- Turmeric contains curcumin, which possesses antidiabetic properties.
- Fruit and vegetables contain fiber, which lowers blood sugars and hemoglobin A1C.
- Stevia from the stevia plant reduces blood sugars following a meal in patients with type 2 diabetes.
In summary, all these substances are examples of triggering epigenetic mechanisms to interfere with the expression of negative health problems where inheritance may also play a role.
Conclusion
This was a whirlwind review of how a healthy diet, supplements, fruit and vegetables, exercise and other healthy lifestyles can overcome genetic and epigenetic traits. After reading about this huge line-up of substances that can contribute to your health, you may feel slightly overwhelmed. Are you going to get all these wonderful items from the health food store and live on a bunch of supplements? Of course this is not the fact! Some herbals can be extremely helpful to combat inflammation, such as curcumin.
The essential facts of treatment of obesity and diabetes
But the most essential fact remains very simple: to cut down sugar and too many starchy foods, as they will trigger repressed genes to cause diabetes, obesity, heart attacks and strokes. We need to inform ourselves and stay vigilant to the fact how toxic foods may be, and we have to cut them out in order to stay healthy. We can become much more resilient to health challenges than we may have thought possible.