Medical news today had an article in October 2023 that reviewed ashwagandha’s benefits. I thought it would be useful to discuss this topic in an abridged version. Often things get distorted on the Internet and a reality check helps to separate facts from fiction. Ashwagandha (botanical name: Withania somnifera) is a small shrub that grows in Southeast Asia, Africa and some areas of India. An alternative name is Indian ginseng. Ashwagandha has been part of Ayurvedic medicine for more than 3000 years.
About ashwagandha’s effectiveness
Ashwagandha is part of natural medicines that go under the name of adaptogens. The effective substances of ashwagandha were isolated. Researchers named them withanolides. They are alkaloids and consist of polyoxygenated steroidal lactones with 28-carbon ergostane skeletons.
People are taking ashwagandha supplements to counter stress and fatigue. But it also increases testosterone, which increases muscle mass. In addition, there is an increase of libido in men as well as in women.
People with insomnia benefit from the relaxing and sleep-inducing effect of ashwagandha supplements. Ashwagandha stimulates the immune system. It also significantly counters the stress response, as it lowers cortisol levels.
The active chemical components of ashwagandha
Various researchers pinpointed the diverse actions of ashwagandha extracts to withanolides, which are the pharmacologically active ingredients. There are at least 25 different chemical structures of withanolides, which are depicted in this reference: This explains the diverse effects of ashwagandha extracts on the immune system, the stress hormone axis, the libido brain centers and testosterone production. One human study showed that within 96 hours of ashwagandha extract administration the immune system was activated; T cells and natural killer cells were measured and were significantly elevated in number in comparison to controls:
Specific clinical trials showing effects of ashwagandha
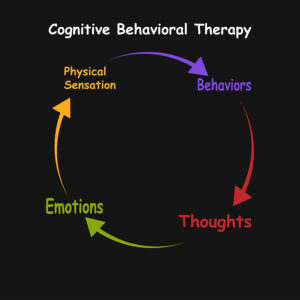
Effects on the brain
In a small clinical study oral intake of ashwagandha improved performance on cognitive tasks, executive function, attention, and reaction time.
Dr. Amala Soumyanath is a professor of neurology in the School of Medicine at Oregon Health & Science University. She stated: “These laboratory studies show that ashwagandha extracts can act on neurotransmitter pathways including those involving serotonin and Gamma-aminobutyric acid (GABA), and also affect systems like the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic-adrenal-medullary (SAM) axis.”
What does this mean? It means that ashwagandha contains a mix of withanolides that calm down the brain, particularly when it is stressed. At the same time, it increases serotonin and GABA, which has antidepressant and calming effects. Clinical trials have measured cortisol levels in volunteers and found that cortisol is lowered within a few weeks. This is the strongest evidence that ashwagandha in fact counteracts stress.
Libido and muscle strength
A small human study found that muscle strength was higher after exposure to oral ashwagandha in comparison to controls.
Ashwagandha showed a significant increase of maximum oxygen consumption (VO2max) in healthy adults and athletes, which is a direct measurement of exercise fitness. A clinical trial with 50 overweight males aged 40-70 years, showed that 16 weeks of oral ashwagandha increased their testosterone level by 14.7%. In addition, there were improvements in fatigue, vigor, and sexual and psychological well-being. There was also an increase of 18% of DHEA-S a precursor of testosterone. The authors felt that a larger study with a longer observation time would be beneficial to confirm this study. Overall, the objective effects of ashwagandha are in the mild to moderate category. The mild increase in testosterone affects libido only marginally. Some articles in social media are vastly exaggerating the objective findings.
Health risk of ashwagandha
There are downsides as well. Ashwagandha stimulates the immune system and in doing so may exacerbate autoimmune diseases. It also can increase thyroid hormones, which is important to know for people with hyperthyroidism or hypothyroidism. Men who have hormone sensitive prostate cancer should avoid ashwagandha, because it elevates testosterone.
Researchers pointed out that gastrointestinal upsets, such as diarrhea, nausea, and vomiting due to ashwagandha are common side effects. The higher the dosage and the longer the exposure is, the more likely it is that the patient experiences side effects. Researchers reported a few cases of reversible liver toxicity cases due to ashwagandha. At this point the effects of concomitant medications taken at the same time as ashwagandha is not known.
Conclusion
Lately social media is full of ashwagandha’s benefits. Rosy reports of increased libido, extra energy and boosts of confidence circulate on the Internet. Men are told that in order to build up muscle bulk with exercise they must take ashwagandha. This review checked the facts. There is a 14.7% rise in testosterone from taking ashwagandha and this may contribute to an increase of muscle mass with exercise, but this is not a huge effect. Also, the mild increase of libido due to the increase of testosterone is not as significant as reported in the social media. The active ingredients of ashwagandha are the withanolides, which researchers isolated. They do help to deal with stress-related problems like lack of energy and insomnia. In addition, they stimulate the immune system to give a stronger response.
Side effects of ashwagandha
But ashwagandha also has some side effects. It can make auto immune reactions worse. It can interfere with both hyperthyroidism and hypothyroidism. Men who have hormone sensitive prostate cancer must avoid ashwagandha because of the testosterone increase. Gastrointestinal upsets, such as diarrhea, nausea, and vomiting from ashwagandha supplementation are common side effects. So far scientific evidence is based on relatively small clinical trials. Scientists must conduct much bigger trials that are going on for several years to provide more in-depth information on the effects of ashwagandha.