This article is about exercise for healthy aging and a young brain. A review article in Medical News Today states that several research papers showed that exercise greatly improves brain health, cognition and mood. It also reduces the risk of neurodegenerative diseases.
The benefits of regular exercise
Here is a list of the beneficial effects of regular exercise:
- Increased muscle strength
- Improved heart health
- Lower blood sugar
- Improved mood
- Alleviates stress
- Improvement of cognitive function
Researchers from Stanford Medicine have examined in a rat model how exactly exercise influences various tissues. Unfortunately, such experiments in humans are not possible and results of rat experiments do not readily translate into the human context. In 8 weeks of regular exercise rats experienced stimulation of the immune system, a reduction of the stress response, an increase of energy production and stimulation of the metabolism. From indirect measurements we know that in humans the same findings likely also hold true. The mitochondria, the area in cells where energy production occurs, are stimulated in muscles, the heart, liver, kidneys, and white adipose tissue.
Effect of exercise on the immune system
Researchers showed in a mouse model that exercise stimulated the T cell response and rejuvenated aging microglia in the brain. The result is a strengthening of the immune system and rejuvenation of the supportive microglia. In the aging human regular exercise rejuvenates microglia in the hippocampus. This can prevent dementia and Alzheimer’s disease.
Exercise strengthens brain cell connections
How does exercise affect the functioning of the brain?
- Synaptic plasticity increases
- Stimulation of blood flow
- Brain-derived neurotrophic factor increases
Ryan Glatt is a senior brain health coach and director of the FitBrain Program at Pacific Neuroscience Institute in Santa Monica. He said: “Exercise enhances synaptic plasticity and blood flow while reducing inflammation and increasing the expression of neurotrophic factors like Brain-derived neurotrophic factor (BDNF). These effects can synergistically improve memory, learning, and overall brain health.”
The best forms of exercise for brain health
Glatt said: “Activities combining physical and cognitive challenges, like dance or tai chi, can be especially effective for certain aspects of brain health.”
Brisk walking is a simple method of exercise. However, we also need isometric exercises, which helps muscle strength and endurance. A good way of combining the two forms of exercise is to regularly go to a gym. Use a treadmill for 30 minutes and then use 30 minutes of a workout with 10 weight machines. Mix this with tai chi or ballroom dancing several days per week. This keeps you mentally and physically fit.
Slow your biological age through the use of the “Essential 8”
Research identified 8 factors that determine how long you live. These 8 factors are what can lower your biological age by 6 years. Here are the 8 factors:
-
Diet
A diet high in fruit, vegetables and lean meats helps you to lower your cholesterol level. In addition, avoid trans fats, fried foods and sugary foods. This helps you to lose weight and prevents Together with regular exercise eating a healthy diet prevents heart attacks and strokes.
-
Activity
The American Heart Association recommends 150 minutes of moderate-intensity aerobic activity per week. Alternatively, 75 minutes of vigorous aerobic activity achieve the same thing. Examples of moderate aerobic activity are a brisk walk, jogging, biking, social dancing and water aerobics. Vigorous aerobic activity involves spinning, running, swimming laps or jumping rope. Exercise reduces blood pressure, blood sugar, and cholesterol. It also helps people to reduce weight.
-
Quit smoking
Smoking cigarettes, vaping or using e-cigarettes causes your body to develop higher blood pressure and damages your blood vessels because of circulating toxins. You also develop shortness of breath from narrowed airways. On the other hand, when people quit smoking, their risk of coronary heart disease drops to half after 1 year.
-
Getting enough sleep
People who don’t get enough sleep at night tend to have higher blood pressures, higher cholesterol and higher blood sugar values. This leads to weight increase and obesity. Sleeping at night for 7 to 9 hours improves cardiovascular health.
-
Body mass index (BMI)
An elevation of your body weight occurs when you eat the wrong foods and combine this with a sedentary lifestyle. Increased weight causes heart and joint problems as well as diabetes. Eating the right foods and exercising regularly gets your BMI into the normal range. This reduces your biological age.
-
Cholesterol
An increase of cholesterol can cause heart attacks and strokes. But when you watch your fat and cholesterol intake you can reduce your cholesterol level. Make healthier choices with foods like reducing saturated fats, reducing refined carbohydrate intake, eating more vegetables and leaner meats. This reduces inflammation in the arteries and plaque deposits with much lower risks of heart attacks and strokes.
-
Blood sugar
Increased blood sugars lead to diabetes. In this case there is accelerated hardening of the arteries in the heart, brain, eyes, and kidneys. This leads to premature heart attacks and strokes. People need to avoid eating refined sugars, carbohydrates (bread, pasta, rice) and sugary drinks. This normalizes blood sugars and your biological age reduces. Regular exercise is also important to burn off any excess sugar in the system.
-
High blood pressure
An elevated blood pressure strains the arteries and the heart. If you don’t pay attention to this you are at a high risk of getting heart failure, a heart attack or a stroke. Sticking to a heart healthy diet, avoiding salty foods, and exercising regularly allows you to lower your blood pressure and avoid the above mentioned complications. If these measures alone do not reduce your blood pressure to normal, ask your doctor to prescribe blood pressure lowering medications for you.
-
Bioidentical hormone replacement
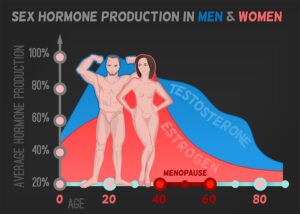
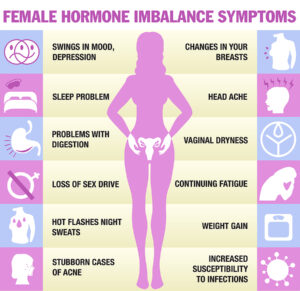
What was not contained in the 8 factors was bioidentical hormone replacement. As you can see from the illustration, testosterone in males reduces more slowly in males (with a delay of 10 years) in comparison to estrogen reduction in menopausal women. Several authors describe that men and women in andropause and menopause live longer when bioidentical hormones are administered compared to those that do not use hormone replacement therapy.
Conclusion
Regular exercise even in older age keeps your brain free from dementia or Alzheimer’s disease. But in addition to this other research showed that 7 more factors are important to reduce your biological age. They are a healthy diet, quitting smoking, getting enough sleep and reducing your body mass index. In addition, you need to keep your cholesterol and blood sugar levels normal. Control high blood pressure with a healthy diet, refrain from salty foods and if necessary, treat it with medication.
Life’s essential 8 factors
It is important to simultaneously control all these “Life’s essential 8” factors for optimal control. People who do this were found to consistently have a lower biological age than others who do not. They also tend to not get Alzheimer’s disease whereas controls do. Lifestyle factors matter for healthy aging and a young brain. Studies showed that the biological age of those who take care of their lifestyles is on average 6 years younger than that of controls. You can reduce your biological age even further with bioidentical hormone replacement in andropause and menopause.