In general, probiotics and a phage blend for digestive problems can help patients with irritable bowel syndrome (IBS). It is important to realize that about ¾ of Americans suffer from digestive problems. They develop symptoms of gas, bloating, diarrhea and stomach pains. To put it another way, about 1 in 7 Americans suffer from the condition, called chronic irritable bowel syndrome. That is to say, he underlying problem is an imbalance of gut bacteria where the bad ones outnumber the good ones. There are a number or reasons why bowel flora gets disrupted. We eat more processed foods, less fiber, and beef products from industry farms contain antibiotic residues. In feedlots for beef cattle antibiotics are fed to the animals as growth promoters. The residues in the meat kill the good bacteria in our guts and the bad ones proliferate. This causes digestive problems, but also weakens our immune system.
How probiotics work
Probiotics can restore our gut flora to a large extent. But some of the probiotic action gets lost in the stomach from the acidic milieu. A recent publication from a panel of gastroenterologists has not supported the wide use of probiotics. They came to the conclusion that probiotics have not shown enough benefit to a number of clinical conditions. The researchers mentioned Crohn’s disease, C. difficile infection, ulcerative colitis and irritable bowel syndrome (IBS) in particular of not responding to probiotics. But this may be because of inactivation of some of the power of the probiotics by stomach acid. In addition, by not using phages to potentiate the probiotic action probiotics may fail to permanently to improve the gut flora. I have previously discussed the importance of probiotics for the gut flora.
History and use of bacteriophages
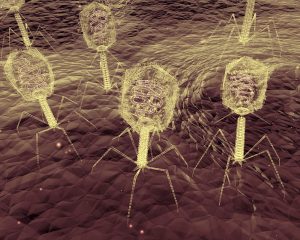
Bacteriophages are now often just called phages. Dr. Frederick Twort, an Englishman detected phages in 1915 during World War I. Essentially a phage consists of either DNA or RNA and a protein envelope around this. Phages are very specific for certain bacterial strains. They attach to the bacteria and inject their own DNA or RNA into the bacteria. This stops the bacteria from multiplying, but makes the bacteria produce many more identical phages. Phages are useful to control the growth of problem bugs including antibiotic-resistant bacteria. However, the regulatory agencies were slow to approve phages despite a good safety record. Life Extension Magazine recently published a review article about this subject.
Phages helping to protect probiotic bacteria
Phages naturally play a role in keeping the gut flora stable. In this lengthy review, published in January 2020 phage actions are reviewed. It also mentions the connection between the gut flora and the immune system. The Life Extension Magazine article mentioned above describes experiments that show the action of phages. E. coli is the main bacterium in the large intestine. It is also the bacterium that can cause pneumonia, diarrhea and urinary tract infections.
Experiments with bacteria and phages in Petri dishes
According to the Life Extension Magazine article researchers did experiments with Bifidobacterium longum, one of the desirable gut bacteria. This was placed on a Petri dish along with E. coli bacteria. In a second Petri dish Bifidobacterium longum, E. coli and a phage mix were placed. After 5 hours there was hardly any growth of Bifidobacterium longum in the first petri dish, as it was crowded out by E. coli. The result in the second Petri dish was interesting: the Bifidobacterium longum colonies were 7000-times higher in number than in the other Petri dish without the phage mixture. The phages had selectively attacked the E. coli bacteria, which made room for the Bifidobacterium longum bacteria to multiply.
Animal experiments with bacteria and phages
The Life Extension Magazine review mentions animal experiments with phages next. One group of mice received B. longum and the disease-causing E. coli in their food. The other group had the same bacteria plus a mix of phages directed against E. coli. For the phage group the results within 24 hours were as follows.
- The E. coli count in the small intestine was 10-fold lower, in the large intestine 100-fold lower and in the fecal matter 100-fold lower.
- The phage group also had a 100-fold increase of the B. longum count in the small intestine. The large intestine also had a 100-fold increase of the B. longum count. And there was a 40-fold increase of B. longum in the fecal matter.
Control mice without the phage mix developed constipation and intestinal segments showed redness, swelling and leaks. In contrast, the phage mix group of mice showed no side effects and had improved digestive function.
Human studies using probiotics and a phage blend for digestive problems
Safety tests of phage therapy were next in 2005 involving 15 volunteers. There were no side effects using two different phage concentrations to diminish E. coli. Researchers had done other safety experiments in Russia and in Poland in the past. Patients with ulcerative colitis responded with improved symptoms and improved endoscopic findings to treatment with two probiotics. They received fermented milk products (Cultura) containing live lactobacilli (La-5) and bifidobacteria (Bb-12) for 4 weeks. There were 51 patients with ulcerative colitis and 10 patients with familial adenomatous polyposis. Abdominal cramps, Involuntary defecation, leakage and the need for napkins were significantly reduced in both groups. An endoscopic score of inflammation showed a significant decreased when the baseline exam was compared to the exam after the 4-week intervention.
Literature review about phages
Here is a thorough review in a publication dated 2011, which describes research from Poland and other countries describing the action of bacteriophages, now simply called phages. It lists many human experiments and shows that phages are safe to use in humans.
Irritable bowel syndrome
Irritable bowel syndrome (IBS) presents with a pathological intestinal function, which can be quite disabling. Another name for it is “spastic colon”, because many patients complain of significant bowel spasms. Some health providers still use this alternative term. This syndrome is more common among women and there is a theory that female hormones may have something to do with the pathophysiology of irritable bowel syndrome. Testosterone on the other hand may have a calming effect on the gastrointestinal tract.
Symptoms and treatment of IBS
Generally speaking, irritable bowel syndrome occurs first in the teens or early twenties, but then frequently tends to become chronic. The patient chiefly complains of abdominal bloating and distension. Bowel movements lead to a marked relief of pain. There is often mucous in the stools. After a bowel movement there is often a feeling that the rectum did not empty entirely, even though it did. Food intake or stress can bring on these symptoms and they always occur during the waking period. At nights most patients have no pain.
Among other measures taking probiotics alone or mixed with phages can normalize the bowel flora. In older men IBS symptoms may indicate a reduction in testosterone production. If the blood contains a low testosterone level, the physician may want to replace the missing testosterone with injections or bioidentical testosterone creams. This can improve IBS in older males.
A safe delivery system for probiotics and a phage blend for digestive problems
Life Extension has developed a dual capsule that brings the inner content safely through the stomach and protects the mix of probiotics and phages from stomach acid. The capsule only opens in the small intestine where it releases its content of probiotics and phages into the gut. This allows the good bacteria like B. longum to multiply and suppresses E. coli, which would otherwise interfere with the beneficial bacteria.
Conclusion
About ¾ of Americans suffer from digestive problems. Many have a disbalance of the gut flora. But it is not easy to replace poor gut flora with a healthy one. Recent research showed that a combination of 7 probiotic strains with a mix of 4 E. coli fighting phages can give tremendous relief from bloating, diarrhea and abdominal cramps to patients with irritable bowel syndrome (IBS). Life Extension has developed a special dual capsule that “sneaks” the capsule through the stomach. It will only open in the small intestine. This way the content of the inner capsule with the mix of probiotics/phages stays safe from the stomach acid. At the end many more beneficial bowel-bacteria are growing in the small and large intestine. This normalizes the symptoms of the patient and leads to better digestion of food. Probiotics and phages are the new players in the gut microbiome.