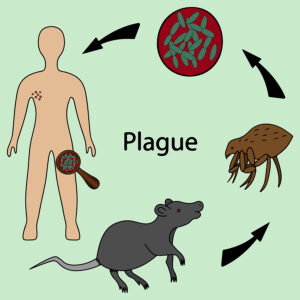
Although the plague is of historic significance, it still is around and the Bubonic plague still affects some people today. In the Middle Ages the world population experienced a reduction from 475 million to 350–375 million between 1346 and 1353. This pandemic relied on fleas on ground rodents, which showed infection with the bacterium Yersinia pestis. Flea bites transmitted the plague bacteria to humans. Nowadays we have effective antibiotics against the plague. Doxycycline is the antibiotic of choice against this bacterium. But in the Middle Ages no antibiotic was available. Those who had a certain variant of the immune system survived, while others who did not have this perished.
Study from nature showing changes of the immune system due to the Bubonic plague
An international research article involving scientists from Canada, the US and France was published in the medical journal nature. Nature published this on Oct. 19, 2022. The title was:” Evolution of immune genes is associated with the Black Death “. The scientists worked with a hypothesis that the human immune genome underwent a shift after the plague in those who survived. They tested their hypothesis by doing DNA analyses in corpses from before, during and after the Black Death. Specifically, more than 300 skeletons came from London/England, where the plague hit hard. 198 samples came from 5 different locations in Denmark. Researchers extracted DNA from the roots of the teeth. They checked for the individual’s’ DNA and for the presence or absence of the bacterium Yersinia pestis. CNN summarized this here.
Results of the study
Hendrik Poinar is a professor of anthropology at McMaster University in Hamilton and coauthor of this study. He said: “It’s a long process, but in the end you have the sequence of those genes for those people from before, during and after the plague and you can ask: Do the genes one population carried look different than the ones another population carried?” There was one particular gene, ERAP2 that had a strong association with the plague. The London study showed that 40% of individuals had an ERAP2 variant protective of the plague prior to the plague. After the plague 50% of the individuals had this variant.
Denmark data
In Denmark prior to the plague 45% of the population carried the variant of ERAP2, while 70% of the population buried after the plague carried this variant. The researchers did in vitro experiments with cultured cells. They could show that macrophages, which are immune cells that initiate immune responses, kill Yersinia pestis bacteria better when the ERAP2 variants are present in comparison to when they are not.
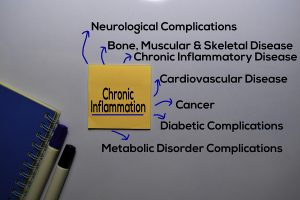
The downside of immunity
The downside of the ERAP2 variant is that researchers linked it to a greater susceptibility to autoimmune disorders. Diseases like Crohn’s disease, rheumatoid arthritis and systemic lupus belong into this category. Luis Barreiro is a professor of genetic medicine at University of Chicago and a coauthor of the study. He said: “This suggests that populations that survived the Black Death paid a price, which is to have an immune system that increases our susceptibility to react against ourselves.” He mentioned further:” It is unlikely that Covid-19 outbreak would shape our immune system in a similar way — largely because the disease predominantly kills people after their reproductive age, meaning it’s unlikely genes that confer protection would be passed on to the next generation.”
Conclusion
A publication in October of 2022 examined 300 skeletons from London, England where the plague hit severely between 1346 and 1353. The study also examined skeletons from Denmark. In both locations the scientists timed the samples before, during and after the pandemic. They found a genetic variant of the immune system by the name of ERAP 2, which changed in the population before and after the plague. The London study showed that 40% of individuals had an ERAP2 variant protective of the plague prior to the plague. After the plague 50% of the individuals had this variant. In Denmark 45% of the population carried the variant of ERAP2, before the plague while 70% of the population buried after the plague carried this variant. In vitro studies showed that macrophages were more aggressive as a result of sensitization of the immune system from an increase of the ERAP2 variant.
Autoimmune diseases
The increase of the ERAP2 variants stimulates the immune system. The researchers determined with in vitro studies that the Yersinia pestis bacterium stimulate macrophages. The downside of the ERAP2 variant is that researchers linked it to a greater susceptibility to autoimmune disorders. Diseases like Crohn’s disease, rheumatoid arthritis and systemic lupus belong into this category. Professor Luis Barreiro from the University of Chicago said:” It is unlikely that Covid-19 outbreak would shape our immune system in a similar way — largely because the disease predominantly kills people after their reproductive age, meaning it’s unlikely genes that confer protection would be passed on to the next generation.”