A new study from the Brock University in St. Catharine’s, Ont. showed that poor diet habits can cause Alzheimer’s. Specifically the risk for Alzheimer’s was a combination of high saturated fats in the diet in combination with too much sugar.
The third triggering factor was the normal aging process that also contributed to the development of Alzheimer’s.
The study showing that poor diet habits can cause Alzheimer’s
Master student Bradley Baranowski and PhD student Kirsten Bott conducted the experiments under the supervision of Assistant Professor of Health Sciences Rebecca MacPherson. The experimental group consisted of middle-aged mice that were observed for 13 weeks. They received a high-fat/high-sugar diet. The control group received a normal diet.
The experimental group with the high fat/high sugar diet was aging prematurely. They also showed elevated inflammatory markers, elevated insulin levels and cellular stress. Dr.MacPherson mentioned that the middle-aged mice would be comparable to humans aged 40 to 60. “[We’re] trying to see what the initiating signals are that can lead to progression of Alzheimer’s disease,” MacPherson said.
Lifestyle choices matter
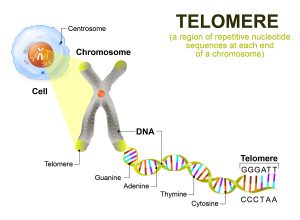
“People often view Alzheimer’s disease as a genetic disease when in fact, genetic mutations leading to Alzheimer’s accounts for less than five per cent of cases,” Baranowski said in the press release. “This study highlights that our lifestyle choices matter and can potentially put us at risk of developing or progressing neurodegenerative diseases such as Alzheimer’s.”
Other studies that support the concept that lifestyles matter
Over the years many other researchers have analyzed what factors contribute to getting Alzheimer’s. It probably is a combination of several factors.
Age
Age is one of the major risk factors. Most Alzheimer’s patients are above the age of 65. Above 65 the risk doubles every 5 years. By the time we are 85 our risk is 1/3 to get it.
Family history
If you have a parent, brother or sister who came down with Alzheimer’s, you have a higher risk of getting it.
Environmental factors
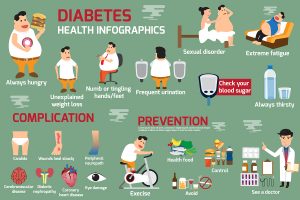
Often environmental factors like eating too much sugar or too much saturated fat are confused with family history factors. Nutritional habits in a family can be like a tradition. It may appear as if this is a family history of Alzheimer’s when in reality poor eating habits were passed on from generation to generation. A lot more research is necessary in this area.
History of Head injury
A history of a closed head injury carries with it a higher risk of Alzheimer’s later in life. We need to use seat belts in cars and helmets when bicycling. Avoid risky sports activities where you would sustain a traumatic brain injury.
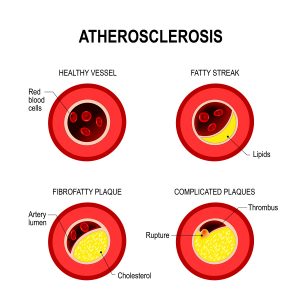
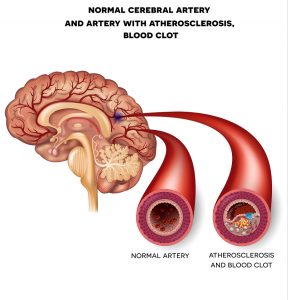
Heart disease
There is a link between heart disease, diabetes, stroke, high blood pressure, high cholesterol and Alzheimer’s. When brain arteries get clogged, the brain deposits more beta-amyloid protein as plaques. This is a sign of early Alzheimer’s disease.
Older Latinos and older African Americans
Older Latinos have a 1 ½-times higher risk than older whites to get Alzheimer’s and dementia. On the other hand older African-Americans are 2-times more likely than older whites to come down with Alzheimer’s. The reason for this is not entirely clear. But a big factor likely is the cardiovascular risk that is higher in Latinos and African Americans. This translates into a higher risk for Alzheimer’s.
Prevention of Alzheimer’s disease
There are more publications that point out that Alzheimer’s disease is largely preventable by cutting out those factors that contribute to its development.
Here is a list of steps to follow in order to prevent Alzheimer’s disease.
- First of all treat diabetes, high blood pressure and obesity aggressively. This eliminates cardiovascular risk factors, which keeps the brain vessels open.
- Furthermore quit smoking. By preserving the cardiovascular system the brain stabilizes.
- Another important factor is physical activity: exercise daily! This maintains cardiopulmonary fitness. It also keeps your brain vessels open.
- Also, take care of your diet: eat balanced meals and avoid junk food. A Mediterranean diet or the MIND diet are examples of diets that help prevent Alzheimer’s. Note that these are low sugar and low saturated fat diets. This fits the initial observation that you read in the beginning of this blog. Mice on a high fat/high sugar diet showed premature aging and developed Alzheimer’s. Knowing this, it is good to do the opposite: cut out excessive saturated fats and sugar. Sugar increase LDL cholesterol and triglycerides, which leads to hardening of arteries.
- Mental stimulation is another important factor for preventing Alzheimer’s. With lifelong bilingualism there was a delay of about 4.5 years in onset of dementia. The ACTIVE study is in the link above. It showed that mental stimulation could indeed delay the onset of Alzheimer’s over a 10-year period.
Conclusion
Above all, I cannot emphasize enough how important a healthy diet is for a healthy mind. The combination of an overabundance of saturated fats and refined sugar was found to be the cause of premature aging in mice. But likewise, we know from human trials that this also causes premature aging in humans and higher incidence of Alzheimer’s. As a result, it is logical to recommend a lower intake of saturated fat and to reduce sugar intake. It will prevent hardening of the arteries and slow down the development of Alzheimer’s.
But there are many other recommendations to avoid getting Alzheimer’s: quit smoking. Stay physically active by exercising daily. Use a Mediterranean diet or the MIND diet to prevent Alzheimer’s. Clinical trials with these diets have shown them to be effective. Treat diabetes, high blood pressure and obesity aggressively as this will stabilize your metabolism. As a result it also prevents Alzheimer’s. Finally, stimulate your brain every day by doing various activities. This forms new synaptic connections inside your brain and postpones Alzheimer’s from setting in as you age.