In the first place, Dr. Joseph Raphaele reviewed why telomeres are important at a Conference in Las Vegas in December 2019. This was at the 27th Annual World Congress on Anti-Aging Medicine in Las Vegas from Dec. 13 to 15, 2019. The actual title of his lecture was: “Telomeres in 2019; clinical developments and cutting-edge applications”.
Notably, Dr. Raphaele reviewed how various animals have quite different life expectancies. First, the Aldabra giant tortoises, for instance can live up to 152 years. Second, the house mouse can at the most live up to 6 years, but its predator, the cat lives up to 38 years. Finally, humans can live up to 122.5 years.That is to say, the average mortality rate doubling curve of man is 8 years. Dr. Raphaele introduced the terms “lifespan” and “health-span”.
Lifespan versus health-span
The first thing to remember is that our lifespan is defined by the number of years we live. On the contrary, the health-span is defined by the number of years you do not have any disease and your physical and mental health are good. Dr. Raphaele explained that for the most part the body’s organs have a limit of functioning after 80. For this reason the kidneys, the maximum heart rate, the maximum breathing capacity and the maximum work rate (oxygen uptake) all decline after the age of 80. It is important to realize that in 1961 Dr. Leonard Hayflick showed that there is a limit of how often cells can divide. After 60 doublings cells in tissue culture either die or just stop dividing. The built-in molecular clock resides in the telomeres. The telomeres are the caps at the end of the chromosomes in the cell’s nucleus.
Telomeres and their function in aging
In a word, what is the function of telomeres? In essence, the telomeres protect the integrity of our genes. For the most part, they protect the chromosomes from deteriorating, prevent DNA fusion and massive instability of the genes. In addition, the telomeres allow the cells to divide in an orderly fashion, but only up to the Hayflick limits. In short, the bottom line is that telomeres prevent cells from mutations of the DNA, from senescence and from death.
Shortening of telomere length with age
Dr. Raphaele said that one of the important findings was that telomere length is shortening with age. Notably, he showed a slide similar to this. To clarify, this graph shows telomere length as a function of the lifespan in years. The telomere length is obtained by a blood test. This determines the length of the telomeres in white blood cells. At a young age it has a length of between 8 and 10 kb. kb stands for kilobase. A kilobase consists of 1,000 pairs of nucleic acid sequences. So, 10 kb means 10,000 pairs of nucleic acid sequences. Around the age of 80 people have much shorter telomeres, only 4 to 6 kb. There is an enzyme, called telomerase that can elongate telomeres by approximately 10%. But this may not be desirable as too much telomerase activation can also stimulate cancer growth.
Age changes telomere length
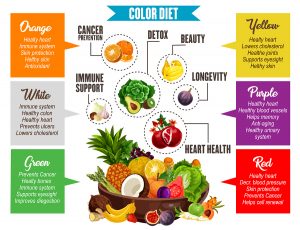
Dr. Raphaele explained further that a telomere loses about 100 base pairs per cell division. But there are other factors that shorten telomeres. Smoking, sedentary lifestyle, high blood pressure, stress and a low antioxidant status all can shorten telomeres. Certain congenital conditions can shorten telomeres by 28%. Dyskeratosis congenita is such a condition where 80% patients die by the age of 30 due to aplastic anemia. This is associated with bone marrow failure. 10% of these patients die from cancer. Apart from age, which shortens telomeres slowly, lifestyle factors are very important. A good lifestyle where you exercise regularly, you don’t smoke and you eat a healthy diet will slow down the shortening of your telomeres. Controlling your stress, sleeping enough hours per night and taking supplements also delays telomere shortening. Certain medications that control diabetes, high blood pressure or thyroid medication that treats hypothyroidism also delay telomere shortening.
Telomeres and shortened lifespan
Researchers could show that good lifestyle practices work by increasing telomerase to a certain degree. This results in lengthening of telomeres and translates into up to 10 years of increased life span. Jerry Shay, PhD said in 2011: “While the aging process is complex and certainly cannot be explained solely on the basis of telomere biology, there is a growing consensus that in some situations telomere biology and telomere tests may have important utility similar to cholesterol assays or blood pressure monitoring measurements.”
Telomeres are not just a biological clock inside our cells. They have a great influence on the function of mitochondria and on how many mitochondria multiply inside cells. This latter process is called mitochondrial biogenesis. In addition, telomeres regulate gene expression.
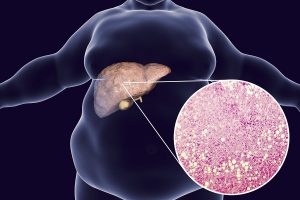
Chronic diseases associated with shortened telomeres
Here is a list of chronic diseases where all the patients have shortened telomeres.
- High blood pressure
- Hardening of the arteries (atherosclerosis)
- Cancer
- Chronic obstructive pulmonary disease (COPD)
- Alzheimer’s disease
- Diabetes and obesity
- Chronic stress
- Metabolic syndrome
Telomeres in cardiovascular disease
Telomere length was found to be shortened in those who developed a heart attack. Researchers compared the telomere length in coronary artery disease (CAD) patients to people with no history of heart attacks. In comparison to this normal group the heart attack victims had telomeres typical for people who are chronologically 11.3 years older than the healthy controls. The researchers calculated that people with telomere shortening had a 3-fold higher risk of coming down with a heart attack.
Telomere length enhancers
- Lifestyle changes can have positive effects on telomere length. Examples are smoking cessation, weight loss and stress reduction.
- Dietary changes: we know that fish oil (omega-3 fatty acids) supplements elongate telomeres as does a low-fat diet.
- Supplements like vitamin D3, antioxidants (vitamin C and E) and astragalus (TA-65) elongate telomeres as well. The astragalus supplement, TA-65 showed a significant elongation of telomeres after 12 months while controls lost telomere length.
- Exercise: in a 24-week experiment of care workers regular aerobic exercise increased the telomeres by 67.3 base pairs.
- Bioidentical hormone replacement in aging people: when hormones are missing after andropause and menopause, the natural hormones need replacing, or the telomeres are shortening.
- High cortisol levels cause telomere shortening.
- Human growth hormone elongates telomeres via telomerase activation.
- The fasting mimicking diet (FMD) was shown to extend life and telomeres as well.
Therapeutic rationale for telomere lengthening in CAD and AD
Patients with coronary artery disease (CAD) are at risk for developing heart attacks and other cardiovascular diseases. Here is an overview of many clinical trials that have been done in humans with CAD. It shows shortening of telomeres in these high-risk patients. But the review also shows that telomeres can lengthen by changing the risk factors of cardiovascular disease. Researchers were increasing the enzyme telomerase that indirectly lengthens telomeres. Both approaches prevent serious cardiovascular disease and increase life expectancy significantly. In severe cases of telomere shortening the physician can consider TERT gene therapy.
Alzheimer’s disease (AD) also is a condition where telomeres are shortened compared to normal controls. Time will tell whether TERT gene therapy is possible to prevent Alzheimer’s disease.
Conclusion
Telomeres are the caps of the chromosomes in our cells. In the past the word “telomere” appeared obscure and only scientists discussed this among themselves. Now we know that telomere shortening is often the reason for chronic illnesses like high blood pressure, hardening of the arteries (atherosclerosis), cancer, chronic obstructive pulmonary disease (COPD), Alzheimer’s disease, diabetes and obesity. Patients who have these conditions often have shortened telomeres in their white blood cells. Over the years we have learnt that lifestyle changes can have positive effects on telomere length. Smoking cessation, exercise, weight loss and stress reduction are elongating telomeres.
Additional factors elongating telomeres
In addition, supplements like antioxidants (vitamin C and E), vitamin D3 and astragalus root (TA-65) elongate telomeres as well. By elongating telomeres, a person can add 10 to 11 years of disease-free life to the normal life expectancy. Researchers showed that telomerase activation by human growth hormone increased telomere length without causing cancer. Dr. Thierry Hertoghe, an endocrinologist from Belgium spoke about HGH replacement in aging people on other occasions. He said that cautiously treating patients with low doses of HGH when blood tests showed deficiency, adds about two decades of life-expectancy to these patients’ lives.